Neuroplastic Approach to Brain and Skull Surgery
At Johns Hopkins, adult and pediatric patients can benefit from a neuroplastic approach when they undergo brain surgery or other types of surgery that may disrupt the contours of the head and face. Instead of correcting the symmetry after the fact, a neuroplastic surgeon and a neurosurgeon working together can prevent the defects in the first place, or work to minimize the risk of complications related to scalp and skull reconstruction.
Prior Deformities and Complications
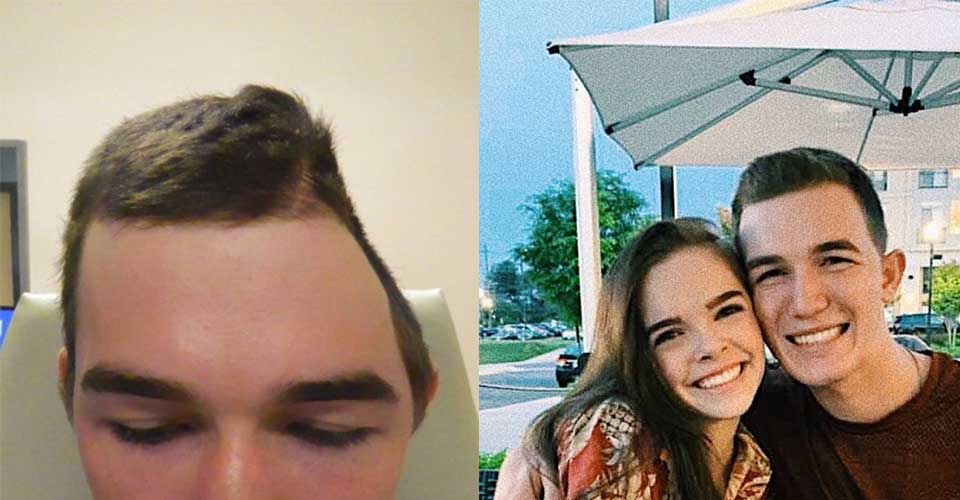
Neuroplastic surgery techniques can benefit patients at any stage of care. Innovative neuroplastic methods can be used to repair complications from prior procedures or address skull deformities that have gone untreated.
-
If you’re unhappy with the shape of your head, consider speaking with a neuroplastic surgeon about your cosmetic procedure options, which use the latest neuroplastic surgery techniques. Altering a delicate structure like the skull requires a careful balance between appearance and function, which a neuroplastic surgeon can effectively navigate.
There is a range of advanced techniques available to safely reshape the contours of your skull to better complement your head and face, including skull implants and skull resection. When needed, the neuroplastic surgery team will work closely with their neurosurgery colleagues to ensure optimal safety from start to finish.
-
Skull deformities — either congenital or acquired later in life — can have a devastating toll on your sense of self. Fortunately, there is a range of techniques available to enhance or restore your appearance.
If a skull defect is harming your confidence and quality of life, consider speaking with a specialized neuroplastic surgical team. Our experts have experience treating a range of skull deformities, including those from:
- Uncorrected craniosynostosis
- Shunt devices for hydrocephalus
- Prior cranial surgeries
- Traumatic head injuries
-
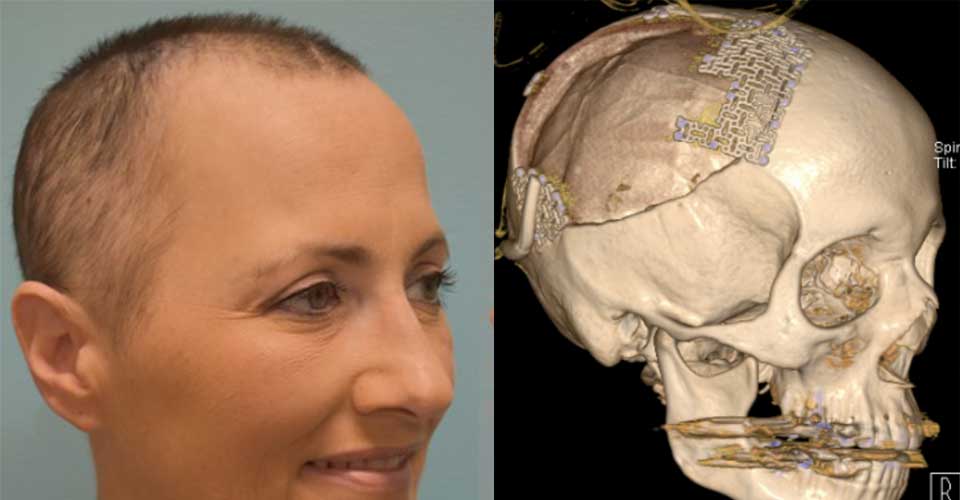
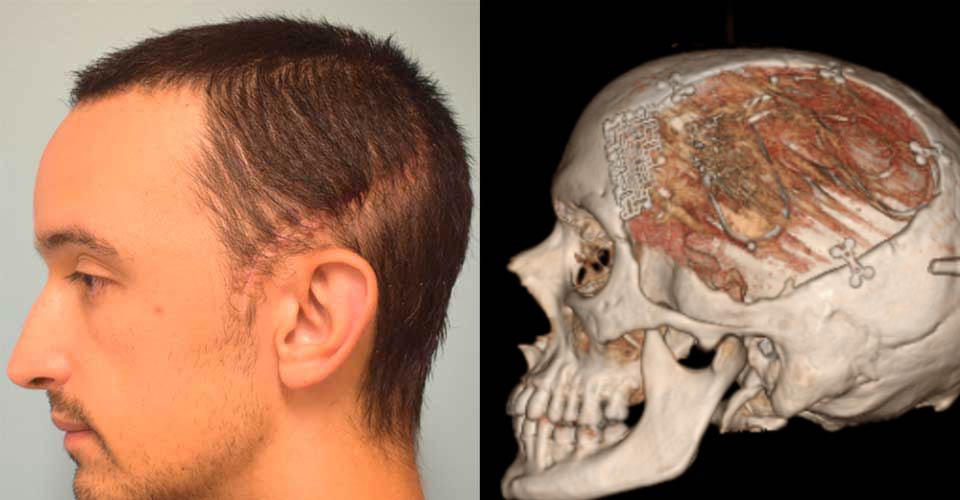
All patients deserve to look and feel their best — no matter what procedure they undergo. For those recovering from a craniotomy, the plates and screws used to repair the skull can cause discomfort, headaches and visible deformities.
Designed to preserve form and function, neuroplastic surgical techniques such as revision cranioplasty offer results that are more comfortable and less noticeable than traditional neurosurgery. Procedures may include removal of hardware, replacement of hardware, or implantation of improved materials with a lower profile.
-
To access the brain, neurosurgeons temporarily remove a piece of bone from the skull. After it’s put back in place with plates and screws, the bone may become infected and/or broken down and absorbed by the body. This complication, while rare, is dangerous and requires specialized expertise to fix. Neuroplastic surgeons, who receive advanced training in scalp and skull care, are uniquely qualified to treat these infections and repair any resulting deformity. Our goal is to identify the exact cause of the skull infection and then prepare an individualized treatment plan, which may involve one or a series of staged surgeries.
If the original bone needs to be replaced, our neuroplastic surgeons can design and insert custom implants that fit seamlessly with the contour of your head.
-
Prominent or poorly healing scalp wounds can significantly affect your health and appearance, and may expose your skull and brain to infection. Often acquired through surgery, these wounds require specialized care from a scalp expert who can safely and effectively manipulate the scalp. This eliminates the need for a more complex procedure like free flap surgery, which is a longer, more invasive operation.
To adequately address the wound and guard against any possible complications in this delicate region, rely on the unique scalp expertise of a neuroplastic surgeon.
Patient Results
Benefits of the Neuroplastic Approach
Neurosurgeons are experts when it comes to the brain, but they rarely have training to care for complications of brain surgery that may affect the appearance of the skull and surrounding soft and hard tissues. When a neurosurgeon works alongside a neuroplastic surgeon, you get the best of both worlds: an effective treatment for your condition and a simultaneous reconstruction of any resulting skull or scalp defects.
A neuroplastic surgeon can help prevent and correct these and other side effects common after certain types of brain and skull surgery:
- Visual narrowing of the head at the temples (temporal hallowing)
- A sunken area in the skull after removing a piece of bone
- An unsightly and/or uncomfortable neurological implant (for managing epilepsy, Parkinson’s disease or other conditions)
What You Need to Know About Neuroplastic Surgery
Johns Hopkins neuroplastic surgeon Chad Gordon describes how patients who need brain surgery can benefit from neuroplastic surgery, a new field that combines the expertise of neurosurgery with plastic and reconstructive surgery to preserve or restore a patient’s appearance.
How do I get treated with the neuroplastic approach?
If you are scheduled for brain surgery at Johns Hopkins, our surgeons will discuss the neuroplastic surgery approach with you during surgery planning. Neuroplastic surgery is built into our process, so you don’t have to request it.
If you are considering another hospital, be sure to ask your neurosurgeon about how he or she plans to avoid or address skull defects. Because neuroplastic surgery essentially combines two or more surgeries into one, it may be a better option regarding recovery, comfort, patient outcomes and cost.