Thyroid Cancer
Overview
What is thyroid cancer?
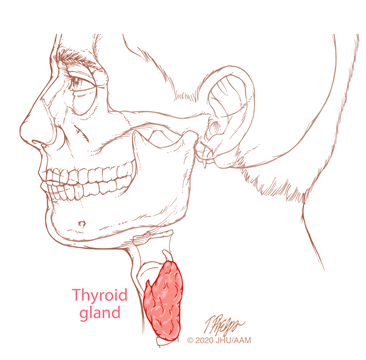
The thyroid gland is located on both sides of the trachea (windpipe) low in the front of the neck. It secretes thyroid hormone, which controls bodily functions such as heart rate, energy level and weight. Another hormone produced by the thyroid gland is calcitonin, which helps the body control calcium balance.
Thyroid cancer occurs in both men and women from the late teens to older ages. It is most common in women between the ages of 30 and 60. Most cases of thyroid cancer occur without obvious cause or risk factors, although some families have inherited forms of thyroid cancer.
Thyroid cancers are categorized by the appearance of the tumor cells on biopsy. The majority of thyroid cancers are called well differentiated thyroid cancers, meaning the cells retain important features of normal thyroid cells when they become malignant. Well differentiated thyroid cancers can be further categorized as papillary thyroid cancer (the most common) and follicular thyroid cancer.
Well differentiated thyroid cancers have an excellent prognosis, and are cured in the great majority of cases. Less common types of thyroid cancer include medullary thyroid carcinoma, poorly differentiated thyroid carcinoma and anaplastic thyroid carcinoma. These types of thyroid cancers are more challenging to manage.
What are symptoms of thyroid cancer?
Most thyroid cancers are asymptomatic. Some can cause symptoms such as pain, difficulty swallowing, enlarged lymph nodes and voice changes. Thyroid cancer is typically diagnosed by discovery of a lump or nodule that is either felt or seen incidentally on ultrasound or another imaging study. A biopsy must be performed to confirm the diagnosis.
How is thyroid cancer diagnosed?
Most thyroid nodules are benign, not cancerous. If a nodule is discovered in the thyroid by physical examination or imaging, it should be further described by the radiologist with attention given to certain details used to estimate the likelihood that a nodule is malignant. An important characteristic is the size of the nodule. Tiny thyroid cancers exist undetected in the glands of as many as one-third of all adults, and the vast majority of these are never detected or cause any clinical problems. For this reason, and because tiny nodules are difficult to biopsy accurately, any nodule of less than 1 centimeter in size may not need to be further evaluated. For nodules of more than 1 centimeter, a grading system is applied and biopsy recommended if the score indicates an appropriate level of concern. Nodules that are not judged to need biopsy may be monitored with repeat ultrasound examinations.
Biopsy can be obtained with a thin needle aspiration under local anesthesia. In many cases ultrasound will be used to verify that the needle actually samples tissue from the nodule. The sample is then evaluated by a cytopathologist. Results may be definitive as showing cancer or certainty of it being a benign nodule, or may be indeterminate. In some cases an additional evaluation by a special laboratory looking at gene changes may be helpful. If needle biopsy is not definitive but clinical features warrant further testing, it may be necessary to remove part of the gland in a surgical procedure to reach a definitive conclusion.
How is thyroid cancer treated?
Treatment usually involves surgery to remove all or part of the thyroid gland. This is performed under general anesthesia with a small incision in the lower neck in most cases. Some select patients with cancer may qualify for trans-oral endoscopic removal. In appropriate cases, lymph nodes are also removed from the neck.
The decision about how much thyroid should be removed is based on several factors that you should discuss with your doctor, including the size of the nodule, your age and gender, and the type of cancer. Most thyroidectomies are accomplished without affecting surrounding structures and function, either as an outpatient visit or with an overnight stay.
After surgery, thyroid hormone may be prescribed to keep the body’s functions in balance. In select cases, additional treatments such as radioactive iodine may be given at an interval after surgery. Standard (external beam) radiotherapy and chemotherapy are infrequently used. Innovative approaches involving immunotherapy, a treatment that uses the body’s immune system to identify and fight the cancer cells, and targeted chemotherapy, which uses medicines to turn off the cancer cells’ ability to grow and spread, may be recommended in some cases.
A diagnosis of any kind of cancer is concerning, but there’s good news! Because most thyroid cancer develops more slowly than other kinds of cancer, it is highly treatable In fact, the chance of surviving 20 years after diagnosis of the most common type, papillary thyroid carcinoma, is 98%.
The Johns Hopkins Thyroid and Parathyroid Center

Our experts provide patients with a personalized treatment plan, tailored to your unique condition and your personal needs. You will benefit from our team of experts, who are at the forefront of diagnosing and treating patients with a variety of thyroid and parathyroid conditions including tumors, nodules and hyperparathyroidism.

