Providing the latest treatments in reconstructive plastic surgery, our experts are available at several convenient locations across Maryland. Our experts also research and implement historic innovations in the most advanced reconstructive transplant procedures including arm, hand, face and penile transplants.
-
Meet Our Surgeons
Our experts specialize in a wide variety of cosmetic and reconstructive plastic surgery procedures.

-
Our Services
See how our team approach helps restore appearance, functionality and mobility.
-
Research
Our experts are at the forefront of discovery in reconstructive transplantation, tissue engineering and more.

Request An Appointment Request An Appointment
Schedule Online Through MyChart
Available for new and follow-up appointments with most providers.
Log into MyChart | Sign up for MyChart
Schedule by Phone

International patients can request an appointment though international patient services.
Pushing the Barriers of Science and Patient Care
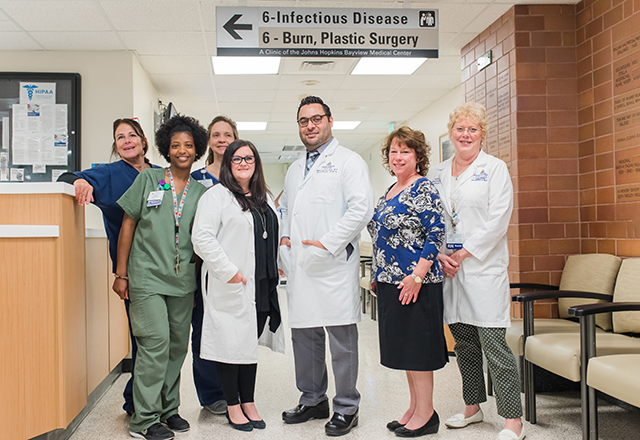
The Johns Hopkins Department of Plastic and Reconstructive Surgery treats adults and children seeking a range of expert care for birth differences, nerve injuries, wound treatment, cancer and trauma reconstruction and more. Our surgeons push the boundaries of science through ongoing research -delivering new treatment options for our patients and elevating standards of care.
Craniofacial Reconstructive Surgery | Restoring Vincent’s Smile
By the time Vincent came to Johns Hopkins for head and neck cancer treatment, he required extensive reconstruction of his jaw and face. A multidisciplinary team that included oral and maxillofacial surgeon Robin Yang, maxillofacial prosthodontist Ghassan Sinada, and plastic and reconstructive surgeon Sami Tuffaha devised an innovative three-part surgery to use his fibula to construct a new upper jaw, in which they mounted dental implants. After being without a smile that he felt comfortable with, Vincent is now able to grin confidently from ear to ear.
The Latest in Plastic and Reconstructive Surgery
-
Reconstructive Surgery After Breast Cancer
Whether it's been 20 days or 20 years since your lumpectomy, you're likely a candidate for reconstruction.

-
Cleft Lip and Palate Treatment
We provide compassionate and expert care that addresses not only the physical, but also the emotional needs, of our patients and their families.

-
Occipital Release Surgery
A first of its kind clinical trial at Johns Hopkins aims to define best practices in occipital release surgery.

Appointment Locations
Our Care Centers
-
The Johns Hopkins Burn Center
Opened in 1968, the Johns Hopkins Burn Center has a long history of providing high quality burn care to patients from Maryland and beyond.
-
Center for Transgender and Gender Expansive Health
The Center for Transgender and Gender Expansive Health provides comprehensive, affirming health care based in the most innovative, researched techniques.










