Rotten Egg Gas Could Guard Against Alzheimer’s Disease
01/12/2021
Typically characterized as poisonous, corrosive and smelling of rotten eggs, hydrogen sulfide’s reputation may soon get a face-lift thanks to Johns Hopkins Medicine researchers. In experiments in mice, researchers have shown the foul-smelling gas may help protect aging brain cells against Alzheimer’s disease. The discovery of the biochemical reactions that make this possible opens doors to the development of new drugs to combat neurodegenerative disease.
The findings from the study are reported in the Jan. 11 issue of the Proceedings of the National Academies of Science.
“Our new data firmly link aging, neurodegeneration and cell signaling using hydrogen sulfide and other gaseous molecules within the cell,” says Bindu Paul, M.Sc., Ph.D., faculty research instructor in neuroscience in the Solomon H. Snyder Department of Neuroscience at the Johns Hopkins University School of Medicine and lead corresponding author on the study.
The human body naturally creates small amounts of hydrogen sulfide to help regulate functions throughout the body, from cell metabolism to blood vessel dilation. The rapidly burgeoning field of gasotransmission shows that gases are major cellular messenger molecules, with particular importance in the brain. However, unlike conventional neurotransmitters, gases can’t be stored in vesicles. Thus, gases act through very different mechanisms to rapidly facilitate cellular messaging. In the case of hydrogen sulfide, this entails the modification of target proteins by a process called chemical sulfhydration, which modulates their activity, says Solomon Snyder, D.Phil., D.Sc., M.D., professor of neuroscience at the Johns Hopkins University School of Medicine and co-corresponding author on the study.
Studies using a new method have shown that sulfhydration levels in the brain decrease with age, a trend that is amplified in patients with Alzheimer’s disease. “Here, using the same method, we now confirm a decrease in sulfhydration in the AD brain,” says collaborator Milos Filipovic, Ph.D., principal investigator, Leibniz-Institut für Analytische Wissenschaften – ISAS.
For the current research, the Johns Hopkins Medicine scientists studied mice genetically engineered to mimic human Alzheimer’s disease. They injected the mice with a hydrogen sulfide-carrying compound called NaGYY, developed by their collaborators at the University of Exeter in the United Kingdom, which slowly releases the passenger hydrogen sulfide molecules while traveling throughout the body. The researchers then tested the mice for changes in memory and motor function over a 12-week period.
Behavioral tests on the mice showed that hydrogen sulfide improved cognitive and motor function by 50% compared with mice that did not receive the injections of NaGYY. Treated mice were able to better remember the locations of platform exits and appeared more physically active than their untreated counterparts with simulated Alzheimer’s disease.
The results showed that the behavioral outcomes of Alzheimer’s disease could be reversed by introducing hydrogen sulfide, but the researchers wanted to investigate how the brain chemically reacted to the gaseous molecule.
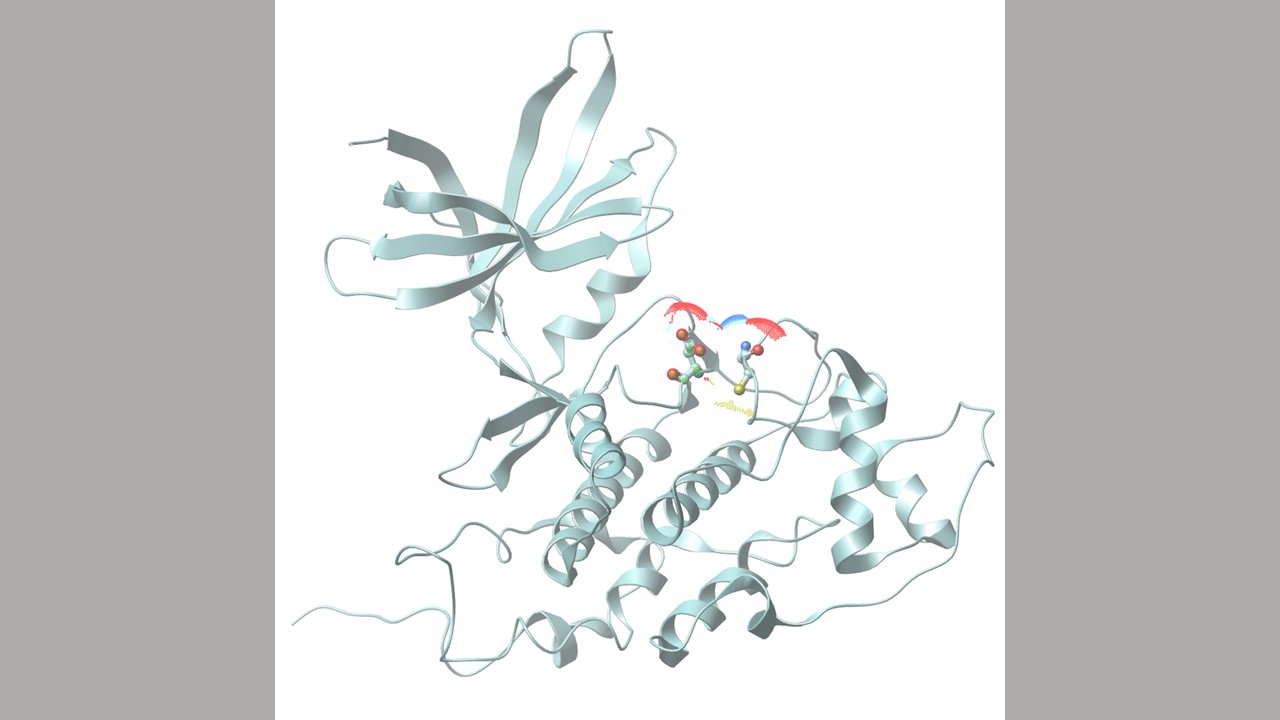
A series of biochemical experiments revealed a change to a common enzyme called glycogen synthase β (GSK3β). In the presence of healthy levels of hydrogen sulfide, GSK3β typically acts as a signaling molecule, adding chemical markers to other proteins and altering their function. However, the researchers observed that in the absence of hydrogen sulfide, GSK3β is overattracted to another protein in the brain called Tau.
When GSK3β interacts with Tau, Tau changes into a form that tangles and clumps inside nerve cells. As Tau clumps grow, the tangled proteins block communication between nerves, eventually causing them to die. This leads to the deterioration and eventual loss of cognition, memory and motor function that is characteristic of Alzheimer’s disease.
“Understanding the cascade of events is important to designing therapies that can block this interaction like hydrogen sulfide is able to do,” says Daniel Giovinazzo, M.D./Ph.D. student, the first author of the study.
Until recently, researchers lacked the pharmacological tools to mimic how the body slowly makes tiny quantities of hydrogen sulfide inside cells. “The compound used in this study does just that and shows by correcting brain levels of hydrogen sulfide, we could successfully reverse some aspects of Alzheimer’s disease,” says collaborator on the study Matt Whiteman, Ph.D., professor of experimental therapeutics at the University of Exeter Medical School.
The Johns Hopkins Medicine team and their international collaborators plan to continue studying how sulfur groups interact with GSK3β and other proteins involved in the pathogenesis of Alzheimer’s disease in other cell and organ systems. The team also plans to test novel hydrogen sulfide delivery molecules as part of their ongoing venture.
Other researchers involved in this study include Biljana Bursac, Thubaut Vignana and Milos Filipovic of the Leibniz-Institut für Analytische Wissenschaften – ISAS and Juan Sbodio, Sumedha Nalluru, Adele Snowman, Lauren Albacarys and Thomas Sedlak of the Johns Hopkins University School of Medicine.
This work was supported by the U.S. Public Health Service Grant (DA044123), the American Heart Association, the Allen Initiative in Brain Health and Cognitive Impairment, the Medical Research Council of the United Kingdom (MR/S002626/1), the Brian Ridge Scholarship, and the European Research Council under the European Union’s Horizon 2020 research and innovation programme (864921).
The Johns Hopkins researchers declare no competing financial interests.
Related Stories:
- More Than Just Jaundice: Mouse Study Shows Bilirubin May Protect The Brain
- New Evidence: How Amino Acid Cysteine Combats Huntington’s Disease
- A New Signaling Pathway Involving the Golgi Apparatus Identified in Cells With Huntington’s Disease
