Curriculum
Year 1: Develop superior clinical skill
| Service | Blocks (2 weeks) | Call Cycle | Patients | Role | Inpatient/Outpatient |
|---|---|---|---|---|---|
| Osler | 8 | Q4 call | GIM | Primary provider | Inpatient |
| Brancati | 1-2 | Days/Nights | GIM | Primary provider | Inpatient |
| MPC | 1-2 | Q3 call | Intermediate | Primary provider | Inpatient |
| MICU | 2-3 | Q3 call | Intensive | Primary provider | Inpatient |
| CCU | 1 | Q3 call | Intensive | Primary provider | Inpatient |
| Oncology | 1-2 | No call | BMT/Solids/Leuks | Primary provider | Inpatient |
| Emergency Department | 1 | No call | Variable | Primary provider | N/A |
| Ambulatory | 6-7 | No call | GIM /Rheum/Endo | Primary provider | Outpatient |
| Vacation | 2 | N/A | 2 two-weeks | N/A | N/A |
Year 2: Explore subspecialty medicine, investigation, and clinical leadership
| Service | Blocks (2 weeks) | Call Cycle | Patients | Role | Inpatient/Outpatient |
|---|---|---|---|---|---|
| Osler JAR (rotation exists first 3 months) | 0-1 | No call | GIM | Teaching/admitting | Inpatient |
| Brancati | 1-2 | No call | GIM | Supervising resident | Inpatient |
| Bayview MICU | 1 | Q3 call | Intensive Care | Primary provider | Inpatient |
| Bayview CCU | 1 | Q3 call | Intensive Care | Primary provider | Inpatient |
| Gen Cards/Cardiomyopathy | 2 | Q4 call | General Cardiology and Heart Failure | Primary provider | Inpatient |
| Polk | 1 | No call | Infectious Diseases | Primary provider | Inpatient |
| MEG (liver) | 1 | No call | Hepatology | Primary provider | Inpatient |
| MPC | 1-2 | Day/Night | Intermediate | Supervisor | Inpatient |
| Carol Johns | 1 | No call | Pulmonary | Primary provider | Inpatient |
| Oncology/Hematology | 1-2 | No call | BMT/Solids/Leuks | Supervising resident/Primary provider | Inpatient |
| Ambulatory | 6-7 | N/A | GIM | Primary provider | Outpatient |
| Elective/Research | 3 | No call | Variable | Variable | Outpatient |
| Jeopardy | 1-2 | Variable | Variable | Variable | Inpatient/Outpatient |
| Vacation | 2 | N/A | 2 two-weeks + 7d winter | N/A | N/A |
Year 3: Become a leader and educator
| Service | Blocks | Call Cycle | Patients | Role | Inpatient/Outpatient |
|---|---|---|---|---|---|
| Osler | 5 | No call | GIM | Teaching | Inpatient |
| JHH MICU | 3-4 | Q3 call | Intensive Care | Supervising resident/Primary provider | Inpatient |
| JHH CCU | 1-2 | Q3 call | Intensive Care | Supervising resident/Primary provider | Inpatient |
| Oncology | 1 | No call | BMT/Solids/Leuks | Supervising resident/Primary provider | Inpatient |
| Supervisor | 0-1 | No call | GIM | Supervising resident | Inpatient |
| Triage | 0-1 | No call | GIM | Triaging resident | Inpatient |
| Emergency Department | 0-1 | No call | Variable | Primary provider | N/A |
| Ambulatory | 6-7 | N/A | Ambulatory Acute Care | Primary provider | Outpatient |
| Elective/Research | 3-4 | No call | Variable | Variable | Outpatient |
| Jeopardy | 1-2 | Variable | Variable | Variable | Inpatient/Outpatient |
| Vacation | 2 | N/A | 2 two-weeks + 7d winter | N/A | N/A |
Inpatient Curriculum
Core Inpatient Rotations
The Osler Medical Service
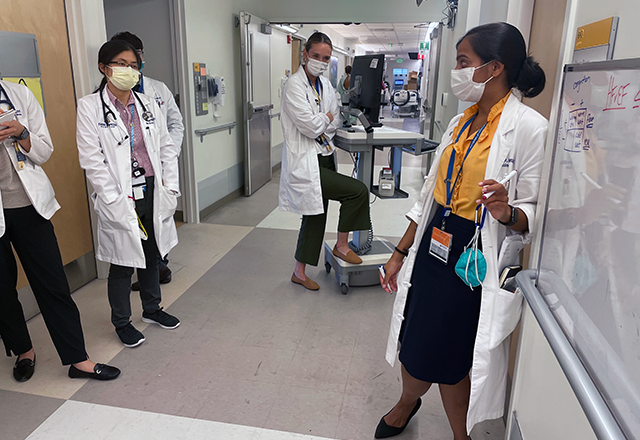
The “O” is the flagship educational experience of the residency program and is modeled after the bedside rounds of Sir William Osler when he founded the program in 1889. Rounds on the Firms occur at the bedside every day. The team consists of four interns, two senior residents and an Assistant Chief of Service (ACS). Interns on the O assume primary ownership of all patients, the seniors lead the team, and the ACS is the attending for the Firm most of the year. The ACS is similar to chief residents in other programs, with two fundamental differences. First, they are at least one year out from internal medicine training so they bring more experiences to the role. Even more importantly--they are the attending most of the year. This allows them to provide unique, year-long, and direct longitudinal mentorship to every intern for the year, compared to a standard model in which interns work with attendings for one to two weeks per year. In addition, the seniors on the O round everyday one-to-one with the ACS to receive personalized leadership training. Teaching on the O is supplemented by expert, diverse and dedicated Firm Faculty.
Brancati (General Medicine)
The Brancati Service is a general internal medicine team that consists of an academic hospitalist attending, two junior residents, and four interns. The team serves as an opportunity for junior residents to develop sophisticated teaching and leadership skills. The team is named in honor of Dr. Fred Brancati, a renowned general internist and former director of General Internal Medicine at Johns Hopkins.
Carol Johns (Pulmonary Medicine)
The Carol Johns Service provides care for general pulmonary, cystic fibrosis, pulmonary hypertension, and lung transplant patients. The team consists of an attending who is a pulmonologist, a pulmonary/critical care fellow, and two junior residents. The service is named in honor of a pioneering pulmonologist and sarcoidosis expert, Carol Johns. The service allows for residents to benefit from outstanding learning opportunities in complex pulmonary medicine and physiology.
Cardical Care Units
Residents in our program rotate in two CCUs, one at The Johns Hopkins Hospital and one at The Johns Hopkins Bayview Medical Center.
In both CCUs our residents learn about myocardial ischemia, cardiogenic shock, arrhythmia, and advanced heart failure management under the direction of leaders in the field. The JHH 12-bed unit cares for a patient population that is highly diverse with a wide breadth of pathophysiology. The team consists of a critical care cardiologist attending, a cardiology fellow, three junior or senior residents, and three interns.
The Bayview CCU team consists of a critical care cardiologist attending, a cardiology fellow, two junior residents from the Osler Program, and two junior or senior residents from the Bayview Internal Medicine Residency.
Hematology
Our unique combined inpatient and consult benign hematology service consists of an attending hematologist and two junior or senior residents. The service allows for exposure to patients with a wide breadth of hematologic diseases including bleeding and clotting disorders, thrombotic microangiopathies, autoimmune cytopenias, bone marrow failure syndromes, myeloproliferative disorders, and sickle cell disease.
Oncology
Through their time on the various oncology services, housestaff learn about the management of malignancies and the complications of oncologic therapies. The services include solid cancer, leukemia, and BMT. Teams consistent of oncology attendings, junior and senior residents, interns and advanced practice providers. In addition to oncology training, residents utilize their critical care skills in a highly complex and sick patient population. End of life issues and palliative care are also emphasized during this rotation.
The Polk Service (Infectious Diseases)
Named after a pioneer in HIV clinical research, B. Frank Polk, the Polk service was founded in 1985 and is one of the premiere inpatient HIV units in the country. Closely connected to the outpatient Bartlett Specialty Practice, the Polk Service provides an unparalleled opportunity to learn about HIV, AIDS, anti-retroviral treatment, and other infectious diseases. The team consists of an infectious disease attending, two junior residents, and at times an infectious disease fellow.
Progressive Cardiac Care Unit (General Cardiology and Cardiomyopathy)
The PCCU has two teaching services for our residents. One is a cardiomyopathy service on which we care for patients with advanced heart failure. This includes substantial exposure to mechanical circulatory support devices and continuous inotropic therapies. The team consists of an heart failure/heart transplant attending cardiologist, a cardiology fellow, and two junior or senior residents. The second service is a general cardiology service, which cares for patients with complicated cardiac conditions other than heart failure. This service exposes residents to management of complicated ischemic heart disease, arrhythmias, and valvular diseases. The team consists of a cardiology attending, a cardiology fellow, and two junior residents.
The Mary Elizabeth Garrett Service (Hepatology)
Named after the forward-thinking founding benefactor of the Johns Hopkins University School of Medicine, Mary Elizabeth Garrett, the MEG service cares for patients with liver disease, including patients with cirrhosis, acute liver injury, liver transplant, and more. The service consists of an attending hepatologist, a gastroenterology/hepatology fellow, and two junior residents. The service allows residents to be exposed to highly complex liver diseases, and to gain unparalleled experience in caring for these patients.
The Medical Progressive Care Unit (MPC)
The MPC is an intermediate care unit, meaning it cares for patients who need a higher level of care than floor care, but who do not require care in the intensive care unit. This service consists of an academic hospitalist attending, three junior residents, and three interns. It provides our junior residents with the experience of leading a team caring for medically complex patients, and allows the entire team to gain important experience in caring for high acuity patients.
MICUs and MICU Triage
Residents in our program rotate in two MICUs, one at The Johns Hopkins Hospital and one at The Johns Hopkins Bayview Medical Center.
In our MICUs, interns and residents learn the latest in the management of critically ill patients with a particular focus on shock, respiratory failure, and mechanical ventilation. The JHH MICU is a 24-bed unit with a diverse patient population that includes general medical critical care to highly complex critical care. There are two MICU teams in the JHH MICU; each is lead by a pulmonary/critical care attending, and includes a pulmonary/critical care fellow, three senior residents, three interns, and advanced practice providers. This integrated structure enables enhanced training and collaboration in teaching and patient care. In addition to the MICU teams, there is a MICU triage resident who focuses on assessing and triaging patients throughout the hospital who may require MICU care, and responding to codes and rapid responses.
The Bayview MICU team cares for a 12-bed unit and consists of a pulmonary/critical care attending, a pulmonary/critical care fellow, two junior residents from the Osler Program, and two junior or senior residents from the Bayview Internal Medicine Residency. The patient population served by this MICU requires highly complex critical care.
Electives
Junior and senior residents enjoy protected elective time, during which they may engage in a research rotation (see research opportunities below), a rotation in any department of medicine subpecialty service at The Johns Hopkins Hospital (inpatient or outpatient), a rotation on our inpatient procedure team, or even create their own experience (provided the experience is approved by program leadership). Some residents also choose to engage in rotations that our Urban Health Residents rotate through as part of their core curriculum or electives. Lastly, residents who are members of one of our Pathways Program engage in pathway-specific electives during their elective time.
Elective time allows for residents to personalize their educational experience while in residency.
Research Opportunities
Our program places a premium on academic pursuit. Each resident may engage in up to 8-weeks of elective time in research. By promoting research and scholarly activities amongst the housestaff, our goal is to cultivate a curiosity and thrill for discovery. Recognizing expert mentorship is essential in these endeavors, we ensure each resident builds a personalized effective network of mentors from across our university. These relationships are facilitated by one-on-one meetings with the Chair of the Department and the Program Director. Our faculty are always excited when an Osler Resident chooses to spend their research time with them. Finally, we are fortunate to have many resources for our residents to pursue research. The Osler Fund for Scholarship assures every resident enough funds to pursue research and to attend national conferences, ideally to present their research. Additionally, we have the Molina and Grasmick Scholars programs which offer funds to residents during their fellowships to pursue fundamental science. More information about this is available on our Physician Scientist Pathway site.
Outpatient Curriculum
Ambulatory Program Overview
Ambulatory Curriculum
Outpatient Experience | Johns Hopkins Osler Medical Residency
Home Visit Program
Goals of Ambulatory Training
The goal of ambulatory training is to give Osler residents the skills to provide the highest quality longitudinal ambulatory care for patients. This is accomplished through the development of clinical expertise, leadership of multidisciplinary teams, and integration of information technology resources and data to inform clinical care decisions. Residents care for their own panel of general internal medicine patients in their continuity clinic as well as see a variety of ambulatory patients in subspecialty clinics. Residents build their panel of primary care patients over the course of three years, allowing them time to develop close relationships with their patients and experience and manage common acute and chronic illnesses.
Patients are seen either in the Johns Hopkins Outpatient Center adjacent to the main hospital or at the East Baltimore Medical Center, an affiliated community clinic that is also a Federally Qualified Health Center (FQHC). In both settings, residents provide a team care approach by working with a team of nurses, medical assistants, case managers, social workers, behavioral therapists, and pharmacists.
Experienced preceptors support the resident practice at each clinical site through teaching, supervising, and mentoring. All residents also work closely over the course of the year with the Ambulatory Assistant Chief of Service (Ambulatory ACS), a recent Osler housestaff graduate who precepts residents at both resident clinic sites and coordinates their ambulatory academic half day curriculum.
Outside of clinic, residents grow their knowledge of outpatient medicine through our multifaceted longitudinal curriculum, which includes academic half days, morning case conferences, and online learning modules. Each time they rotate on ambulatory block, residents attend one or two half-day teaching sessions, which consist of high-yield resident- and faculty-led presentations, hands-on skill-building workshops, and case-based diagnostic reasoning sessions. Topics covered during this protected learning time range from cardiac risk stratification and osteoporosis to primary care psychiatry and gender-affirming care. These sessions are paired with independent learning through a Hopkins-developed, nationally recognized online curriculum.
Each resident can access quality measures for their personal patient panel via a custom-built dashboard integrated into our electronic medical record. This allows residents to see which patients may need to be targeted for outreach, whether to optimize management of their chronic conditions, complete cancer screens, or administer vaccinations.
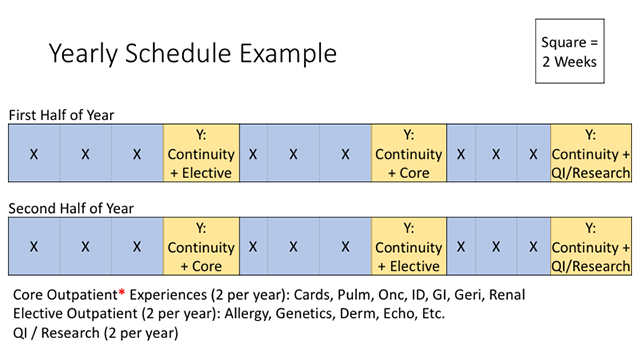
Ambulatory Curriculum
All housestaff are grouped into Firm Teams of four or five residents. This system facilitates a high degree of patient-provider continuity and facilitates the management of any patient care needs that may emerge while the assigned primary care resident is on an inpatient block or vacation.
With the X+Y schedule, following six weeks of primarily inpatient experiences (X), all housestaff transition to two weeks of ambulatory time (Y). Over the course of the year, everyone will have six of these two-week ambulatory experiences. During each Y block, residents spend approximately half of their time in their own primary care continuity clinics and the other half on either quality improvement (QI) or research projects or outpatient specialty experiences.
During the first year, the initial two-week ambulatory rotation is a dedicated immersion block that blends outpatient primary care with curated didactic sessions that focus on the fundamentals of outpatient internal medicine. During subsequent blocks, in addition to continuing with their own primary care sessions, interns are embedded in outpatient endocrinology, geriatrics, and rheumatology clinics.
During their second and third years, residents choose from a broad range of outpatient experiences that are paired with their continuity clinic. Some of our many options include medicine subspecialty clinics (hematology, allergy/immunology, etc.) policy electives (Baltimore County Health Department), and various other clinical opportunities (intensive primary care, sports medicine, transgender care).
Electives
Junior and senior residents enjoy protected elective time, where they may engage in a research rotation (see “research opportunities below”), a rotation in any department of medicine subspecialty service at The Johns Hopkins Hospital (inpatient or outpatient), a rotation on our inpatient procedure team, or even create their own experience (provided the experience is approved by program leadership). Some residents also choose to engage in rotations that our Urban Health Residents rotate through as part of their core curriculum or electives. Lastly, residents who are members of one of our Pathways Program engage in Pathway-specific electives during their elective time.
Elective time allows for residents to personalize their educational experience while in residency.