What Is Afib?
Afib stands for atrial fibrillation (AF), which is a type of arrhythmia, or abnormal heartbeat. Afib is caused by extremely fast and irregular beats from the upper chambers of the heart (usually more than 400 beats per minute).
A normal, healthy heartbeat involves a regular contraction of the heart muscle. A contraction happens about once per second at rest and increases with exercise. Each contraction pushes blood from the atria (the two upper chambers) to the ventricles (the two lower chambers). The ventricles then contract and push the blood to the lungs or to the rest of the body.
But in a person with Afib, faulty electrical signals make the atria contract irregularly and much faster than normal. The atria then get out of sync with the ventricles. Blood can pool in the atrium, which may lead to blood clots and strokes. Afib that causes the lower chambers to beat too quickly can cause heart failure.
Afib may occur occasionally, or it can be constant.
What happens during atrial fibrillation?
A normal heartbeat begins with one electrical impulse from the sinus node, a single point in the heart’s right atrium. A healthy person’s heart usually beats 60 to 150 beats per minute.
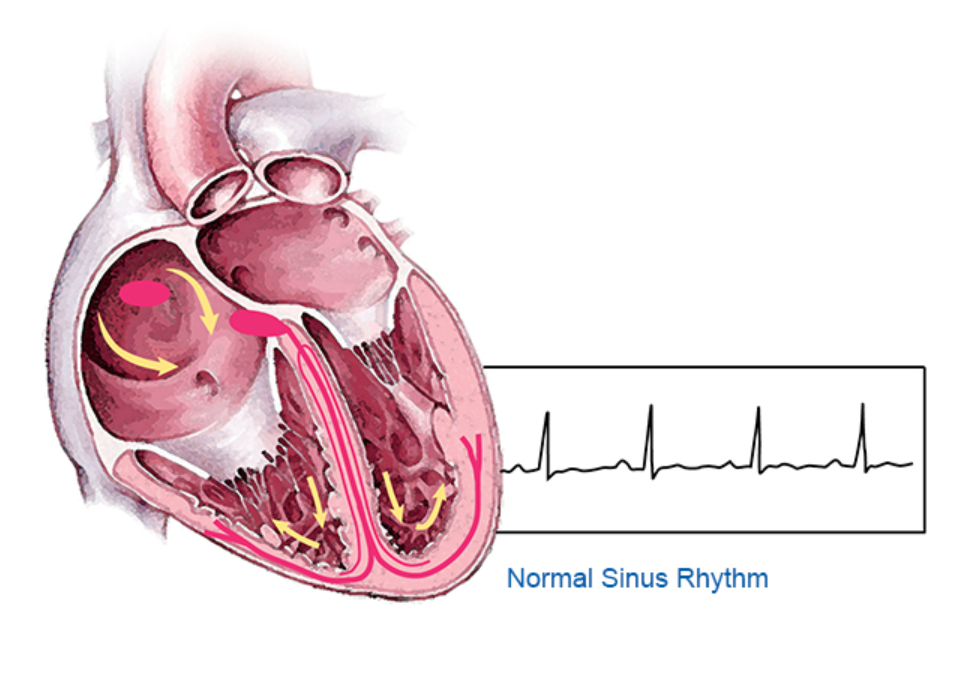
With Afib, electrical impulses fire from multiple sites in both atria. That can cause the atria to contract 400 or more times per minute. The ventricles become overwhelmed trying to keep up with the contractions. They beat faster than they should, and they may not have time to fill with blood and pump blood normally.

As a result, blood pools in the atria instead of moving into the ventricles and out to the rest of the body. This pooling increases the risk of blood clots in the heart. Blood clots can travel from the heart into the bloodstream and into the brain, leading to a stroke.
What are the types of Afib?
There are three types of atrial fibrillation:
- Paroxysmal Afib: This type of Afib occurs intermittently and stops on its own within seven days.
- Persistent Afib: This type of atrial fibrillation lasts longer than seven days. Unlike paroxysmal Afib, it may require cardioversion (electric shocks to the heart) to restore normal rhythm.
- Long-standing persistent Afib: This is similar to persistent Afib, but lasts longer than a year.
What are the symptoms of atrial fibrillation?
Sometimes Afib causes no symptoms at all; you might not know you have it. When it does cause symptoms, those can include:
- Angina (chest pain caused by a reduced blood supply to the heart muscle)
- Dizziness
- Fainting (syncope)
- Fatigue
- Palpitations (feeling like the heart is fluttering or racing)
- Weakness
- Shortness of breath
Afib can also lead to serious complications:
What are the risk factors for Afib?
Afib occurs more often in people with certain characteristics:
- Age older than 50 years
- Alcohol use
- Heart failure
- High levels of stress
- High blood pressure
- Male gender
- Obesity
- Sleep apnea or poor sleep
- Tall height
- Thyroid disease
The condition can run in families, especially when it happens at a young age.
What is Afib with RVR?
Some cases of Afib involve atrial fibrillation with rapid ventricular response (RVR). This is when the rapid contractions of the atria make the ventricles beat too quickly. If the ventricles beat too fast, they can’t receive enough blood. So they can’t meet the body’s need for oxygenated blood. This can lead to heart failure.
How is Afib diagnosed?
If doctors suspect an Afib diagnosis, they’ll perform a physical exam, including a check of the heart rate and rhythm. They will also order an electrocardiogram (ECG or EKG), the definitive test for atrial fibrillation diagnosis.
ECG uses round sensors (electrodes) placed on the chest, arms and legs. Wires connect the sensors to a machine that measures electrical currents in your body. The results provide information about:
- Heart rate and rhythm
- How the heart’s electrical signals travel
- Which parts of your heart are triggering contractions
Because Afib can come and go, a single ECG may not detect a problem. Your doctor may recommend a special ECG monitor to record your heart rhythm over an extended time. Examples include:
- Holter monitor: A Holter monitor is a portable ECG you wear continuously for up to a week.
- Event monitor: An event monitor is a portable ECG you wear for one or two months. It records activity only when it detects an abnormal rhythm or when you manually activate it.
- Implantable monitor: A surgeon can place a tiny implantable monitor under your skin to detect rare Afib events.
- Consumer devices: A number of devices allow people to monitor their own heart rhythms. These include smartphone apps and smart watches.
AFib Treatment at Johns Hopkins
- Heart disease specialists oversee your care.
- Treatments are informed by the latest research.
- Care available throughout the Baltimore and Washington, D.C., metro areas.

How is Afib treated?
The most important step in Afib management is assessing a person’s risk of stroke. For people with multiple stroke risk factors (for example, older than 65 and high blood pressure), anticoagulation medications are recommended. These drugs help prevent blood clots to lower the risk of stroke.
The second step is to slow the person’s resting heart rate to 80 beats per minute. This can be accomplished with medications.
The third step involves deciding whether to control heart rhythm with antiarrhythmic medication or a medical procedure. For people who are in Afib all the time, cardioversion (electrical shock) can restore normal rhythm. Medications or catheter ablation can then help maintain the rhythm.
Medications to control heart rate and rhythm and prevent complications include:
Medications to slow the heart rate:
- beta blockers
- calcium channel blockers
- digoxin
Medications to control heart rhythm (anti-arrhythmics):
- amiodarone
- dofetilide
- dronedarone
- flecainide
- propafenone
Medications to prevent blood clots and strokes (anticoagulants or blood thinners):
- apixaban
- dabigatran
- edoxaban
- rivaroxaban
- warfarin
If medications don’t control Afib well enough to prevent complications, your health care provider may recommend surgical procedures to treat the condition:
- Catheter ablation: Radiofrequency waves, extreme heat or extreme cold are used to destroy the tissue causing Afib.
- A maze procedure: A surgeon makes cuts in strategic places to create a “maze” of scar tissue to prevent electrical signals from passing through.
Learn more about other arrhythmias.