Metastatic Brain Tumors
Featured Expert:
When cancer that began somewhere else in the body spreads to the brain and causes a mass or brain tumor, it’s called metastatic brain cancer. The resulting tumors are called brain metastases or “brain mets.” Johns Hopkins neurosurgeon Chetan Bettegowda offers insight into metastatic brain cancer and the treatment options.
What You Need to Know
- Metastatic brain cancer (also called secondary brain tumors) is caused by cancer cells spreading (metastasizing) to the brain from a different part of the body.
- The most common types of cancer that can spread to the brain are cancers of the lung, breast, skin (melanoma), colon, kidney and thyroid gland.
- Metastatic brain tumors are five times more common than primary brain tumors (those that originate in the brain).
- Metastatic brain tumors can grow rapidly, crowding or destroying nearby brain tissue. Sometimes a patient may have multiple metastatic tumors in different areas of the brain.
What happens when cancer spreads to the brain?
Cancer cells can break away from the primary tumor and travel to the brain, usually through the bloodstream. They commonly go to the part of the brain called the cerebral hemispheres or to the cerebellum, where they form a mass.
Some metastatic brain tumors appear many years after the primary cancer. Others metastasize so quickly that they are identified before the primary cancer.
When the cancer cells reach the brain and form a tumor, it may lead to a variety of symptoms that can be shared by nonmetastatic brain tumors as well.
What are the symptoms of brain metastases?
Common signs and symptoms of brain metastases include:
- Headaches
- Seizures
- Weakness in the arms or legs
- Loss of balance
- Memory loss
- Speech disturbance/problems talking
Other symptoms may include:
- Behavior and personality changes
- Blurred vision/vision disturbance
- Numbness
- Hearing loss
Who is at risk of developing metastatic brain cancer?
About one-third of patients with another type of cancer will develop one or more metastatic brain tumors. The risk for metastatic brain tumors begins to increase after age 45, and is highest in those over 65.
How are metastatic brain tumors diagnosed?
Metastatic brain and spine tumors are not usually diagnosed until symptoms appear. Here are some ways doctors may diagnose a metastatic brain tumor:
- Physical exam: After gathering information about your symptoms and personal and family health history, the doctor proceeds with a physical exam and vision and reflex tests.
- Neurological exam
- Computed tomography (CT or CAT scan)
- Magnetic resonance imaging (MRI)
- Diffusion tensor imaging (DTI) is a type of MRI that visualizes how water molecules pass through parts of the brain. It reveals microscopic differences of tissue structure, including very early infiltration of cancer cells.
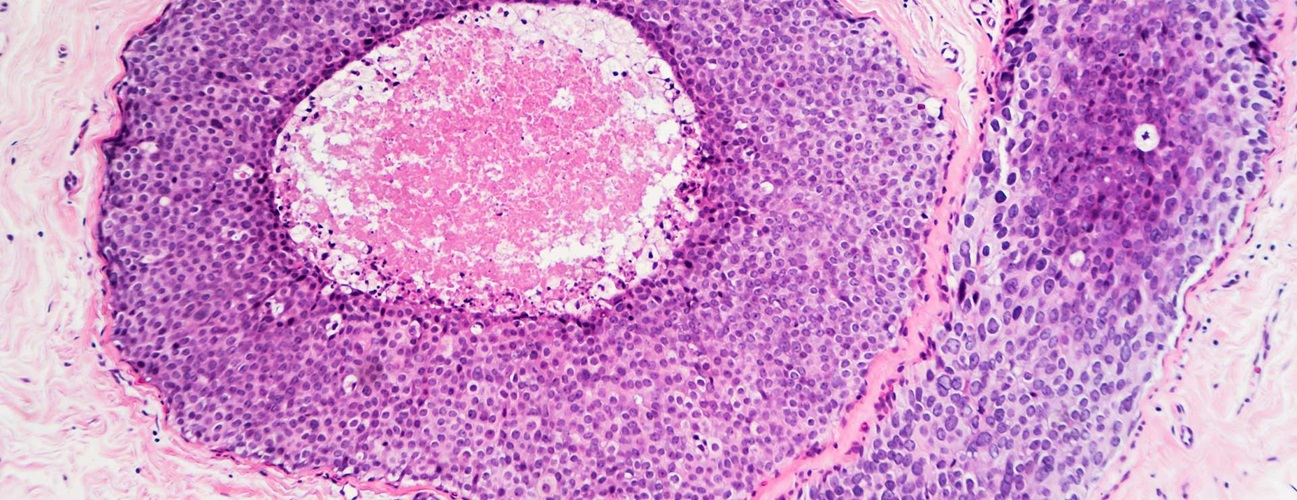
- Biopsy: Collecting a piece of the tumor through surgery may be necessary when the diagnosis is unclear based on the other tests.
Metastatic Brain Cancer Treatment
It is important to know that metastatic brain tumors are often treatable, and can be well-controlled. Generally, the faster you start treatment, the better the chances of killing or controlling the disease.
The treatment options for brain metastases may include:
- Surgery
- Radiation therapy
- Chemotherapy
- Targeted drug treatments
- Immunotherapy
- Clinical trials
In many cases, surgery or radiation therapy can improve — or entirely get rid of — symptoms. Read more about brain tumor treatment.
Metastatic Brain Tumor Surgery
Surgery provides fast relief of “mass effect” — pressure inside the skull resulting from a growing metastatic tumor and swelling of the brain. Some patients may find improvement of symptoms as early as within hours of surgery if mass effect is what is causing your symptoms.
The goal of surgery is to minimize the amount of space the tumor takes up by debulking, which means removing as much of the tumor as possible while maintaining neurological function.
In general, doctors recommend surgery for metastatic brain cancer when:
- There is a clear link between the symptoms and the tumor’s location.
- The primary cancer is treatable and under control.
- The tumor can be safely removed.
The most common type of surgery to remove metastatic brain tumors is called a craniotomy, which can be performed through a variety of approaches, including the keyhole craniotomy.
Learn more about brain tumor surgery and recovery.
Radiation Therapy for Metastatic Brain Tumors
Radiation therapy treats metastatic brain tumors by using X-rays and other forms of radiation (light energy) to destroy cancer cells or prevent a tumor from growing. It is also called radiotherapy.
These painless treatments involve passing beams of radiation through the brain, which can treat cancers in areas that are difficult to reach through surgery. Procedures may include any one or a combination of the following:
- External beam radiation therapy delivers radiation from a machine and through the body to reach metastatic tumors.
- Whole-brain radiation targets the entire brain to hit multiple tumors or any metastatic disease that hides from an MRI scan.
- Stereotactic radiosurgery (e.g., Cyberknife) directs a high dose of radiation targeted to the specific shape of the tumor, sparing surrounding healthy tissue from unnecessary radiation exposure.
- Proton therapy uses protons (instead of X-rays) to treat metastatic brain tumors. Like stereotactic radiosurgery, proton therapy minimizes harm to healthy tissue surrounding a tumor.
- Brachytherapy is radioactive material implanted within a tumor to prevent further growth.
These procedures may be performed after surgery to prevent tumors from recurring at the surgical site and growing into other brain tissue.
Choosing radiation therapy is complex, and often involves working closely with your care team. For some people, stereotactic radiosurgery may offer a better prognosis than surgery. Others may receive whole-brain radiation or a combination of both therapies. You will have a risk-benefit conversation with your radiation team to weigh the potential benefits against the possible risks and side effects.
Because radiation therapy has been so successful in treating brain metastases — and because many live long lives after treatment — studies are now looking at how to manage the long-term effects of treatment.
Chemotherapy for Metastatic Brain Tumors
Because traditional chemotherapy cannot cross the blood-brain barrier, newer treatments called targeted therapy are used as the primary type of chemotherapy for treating metastatic brain tumors.
These drugs identify and attack cancer cells (the target) with minimal harm to normal cells while preventing the growth and spread of cancer cells. Targeted therapy can be administered after surgery or in conjunction with radiation therapy to destroy remaining cancer cells.
Targeted therapies used to treat metastatic brain tumors include:
- Trastuzumab for breast cancer that has spread to the brain
- Erlotinib for the most common type of lung cancer (non-small cell lung cancer) that has spread to the brain
Immunotherapy for Metastatic Brain Tumors
Cancer immunotherapy is a fast-growing field of research that seeks to develop drugs, vaccines and other therapies that trigger the immune system’s natural abilities to fight cancer. Many immunotherapy drugs for metastatic brain tumors act as “checkpoint inhibitors.” Normally, tumor cells can evade attack by activating certain proteins (called checkpoint proteins) that disarm your immune system. Checkpoint inhibitors prevent tumor cells from exploiting this process.
Immunotherapy drugs to treat metastatic brain tumors include:
- Atezolizumab
- Ipilimumab
- Pembrolizumab
- Nivolumab
Clinical trials for new treatments
Researchers are always finding new ways to treat metastatic brain tumors. These new methods are tested in clinical trials. Talk with your health care provider to find out if there are any clinical trials you should consider.
Johns Hopkins Comprehensive Brain Tumor Center
Every metastatic brain tumor, and every patient, is different. The specialists at Johns Hopkins take the time to determine which treatment or combination of treatments will be the most effective for you.
How do you decide which metastatic brain cancer treatment is right for you?
Your neurosurgeon will discuss the most appropriate treatment approach with you by considering these and other factors:
- The type of primary cancer, your response to treatment and current status
- The location and number of metastatic tumors within the brain or spine
- Your general health and preferences regarding potential treatment options
- Your current symptoms
Along with benefits, doctors also consider the potential risks and side effects of any treatment. Many patients are worried about the effects of radiation. Others hesitate about the idea of surgery. Tell your doctor about your concerns — they are important to consider.
Metastatic Brain Cancer Prognosis
Prognosis for metastatic brain cancer varies greatly. Keep in mind that each patient is unique, and with newer treatments, many patients live longer. Speaking with your care team about your unique diagnosis can provide an accurate prognosis.
Palliative Care at Johns Hopkins
Palliative care is specialized medical care that helps patients facing serious illnesses and their families by adding an extra layer of support.
Palliative care teams can help with the symptoms and the stress of living with a serious illness, including controlling pain, providing support for the mental and emotional effects of an illness, and managing other symptoms.