Thoracic Aortic Aneurysm
What You Need to Know
- Most patients with thoracic aortic aneurysms do not have any symptoms; they are usually diagnosed on imaging studies performed for another reason.
- Uncommonly, large thoracic aortic aneurysms may cause back or chest discomfort.
- Diagnosing requires a CT scan and regular CT scans every 6 months or one year to monitor for growth.
- Treatment may include minimally invasive surgical techniques such as stenting.
- Occasionally, a more complex open surgery to replace the affected portion of the aorta is required.
What is a thoracic aortic aneurysm?
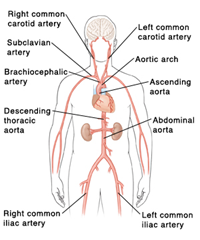
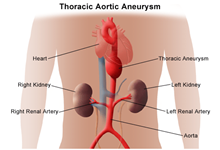
The aorta is the largest blood vessel in the body. It brings oxygenated blood from the heart to the rest of the body. An aortic aneurysm is a bulging, weakened area in the wall of the aorta. Over time, the blood vessel swells. Then it is at risk for bursting (rupture) or separating (dissection). This can cause life-threatening bleeding and possibly death.
A thoracic aortic aneurysm occurs in the part of the aorta that runs through the chest. Aneurysms occur more often in the part of the aorta that runs through the belly or abdomen (abdominal aortic aneurysm).
Once formed, an aneurysm will slowly get larger and weaker. Treatment may include surgery to fix or remove the aneurysm. Or a metal mesh coil (stent) may be inserted. This is to support the blood vessel and prevent rupture.
What causes a thoracic aortic aneurysm to form?
Different diseases that can cause thoracic aortic aneurysms include:
-
Degenerative disease that causes breakdown of the aortic wall tissue
-
Genetic disorders
-
Family history
-
High cholesterol blood levels
-
Plaque buildup (atherosclerosis)
-
Infection (rare)
-
Inflammation of the arteries (vasculitis)
-
Uncontrolled hypertension (high blood pressure)
-
Smoking
What are the symptoms of a thoracic aortic aneurysm?
Thoracic aortic aneurysms may not cause symptoms. When symptoms do occur, they may be linked to:
-
The aneurysm's location and size
-
How fast the aneurysm is growing
-
If the aneurysm has burst or dissected
Sudden, severe pain linked to a thoracic aneurysm may be a sign of a life-threatening medical emergency.
Symptoms of a thoracic aneurysm may include:
-
Pain in the jaw, neck, or upper back between the shoulder blades
-
Pain in the chest or back
-
Pain that seems like a heart attack
-
Wheezing, coughing, or shortness of breath caused by pressure on the windpipe (trachea)
-
Hoarseness as a result of pressure on the vocal cords or nerves leading to the vocal cords
-
Trouble swallowing due to pressure on the food pipe (esophagus)
These can be caused by other conditions. Get medical care right away if you think you have an aneurysm.
How is a thoracic aortic aneurysm diagnosed?
Your healthcare provider will do a complete health history and physical exam. Other possible tests include:
-
Contrast-enhanced CT scan. This test uses X-rays and computer technology to make detailed images of any part of the body. This includes the bones, muscles, fat, and organs. CT scans are more detailed than standard X-rays. Contrast (dye-like substance) will be given through a vein to help make the images more detailed.
-
MRI. This test uses a combination of large magnets, radio waves, and a computer to make detailed images of organs and structures within the body without using X-rays.
-
Echocardiogram. This test is also called an echo. It evaluates the heart’s structure and function. It uses sound waves recorded on an electronic sensor. This makes a moving picture of the heart and heart valves, as well as the structures within the chest. These include the lungs and the area around the lungs and the chest organs.
-
Transesophageal echocardiogram (TEE). This test uses echocardiography to check for an aneurysm and check the heart valves. It can also see if there is a tear in the aorta lining. TEE is done by inserting a probe with a transducer on the end down the throat.
-
Chest X-ray. This test uses invisible electromagnetic energy beams to make images of internal tissues, bones, and organs onto film.
-
Arteriogram (angiogram) . This is an X-ray image of the blood vessels that is used to assess conditions. These include aneurysm, narrowing of the blood vessel, or blockages. Contrast (a dye-like substance) is injected through a thin, flexible tube placed in an artery. The contrast makes the blood vessels easy to see on an X-ray.
How is a thoracic aortic aneurysm treated?
Treatment may include:
-
Monitoring with CT or MRI. These tests are done to check the aneurysm’s size, how fast it’s growing, and the aortic valve.
-
Managing risk factors. Making some lifestyle changes may help control the progression of the aneurysm. These include quitting smoking, controlling blood sugar if you have diabetes, losing weight if overweight, controlling blood pressure, exercising, and eating a healthy diet.
-
Medicine. Used to control factors such as high cholesterol or high blood pressure.
-
Surgery.
-
Thoracic aortic aneurysm open repair. The type of surgery will depend on the location and type of aneurysm, and your overall health. For an aortic root, ascending aorta, or aortic arch aneurysm, 1 large cut (incision) may be made through the breastbone. The aneurysm is removed and a graft placed. If an ascending aneurysm involves damage to the aortic valve of the heart, the valve may be fixed or replaced during the procedure. For a thoracic descending aneurysm, 1 large cut may be made. It may go from the back under the shoulder blade, around the side of the rib cage, to just under the breast. This lets the surgeon see the aorta directly to fix the aneurysm.
-
Thoracic endovascular aortic repair (TEVAR). TEVAR needs only small cuts in the groin. The surgeon uses X-ray guidance and special tools. Then they can fix the aneurysm by inserting a metal mesh coil (stent-graft) inside the aorta. Not all thoracic aneurysms can be fixed with TEVAR.
-
A small aneurysm or one that doesn't cause symptoms may not need surgery until it reaches a certain size. Or until it's quickly growing over a short time period. Your provider may advise watchful waiting. This may include having a CT scan or MRI and echocardiogram scan every 6 months or yearly to closely watch the aneurysm. Blood pressure medicine may be used to control high blood pressure.
If the aneurysm is causing symptoms or is large, your provider may advise surgery.
What are the possible complications of a thoracic aneurysm?
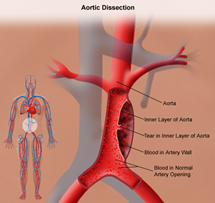
A serious complication of a thoracic aortic aneurysm is an aortic dissection. This is a tear in the aortic lining. It can occur anywhere along the aorta. It starts with a tear in the inner layer of the aortic wall of the thoracic aorta. Blood leaks between the layers. This can be a life-threatening emergency. The most common symptom of an acute aortic dissection is sudden, severe, constant chest or upper back pain. This is sometimes described as ripping or tearing. The pain may move from 1 place to another.
An aortic aneurysm may burst. This is accompanied by blood in the chest. It's a life-threatening emergency
When a diagnosis of aortic dissection is confirmed, surgery or stenting is often done right away. Talk with your healthcare provider about how you can manage your thoracic aortic aneurysm and reduce your risk for complications.
What is aortic dissection?
An aortic dissection starts with a tear in the inner layer of the aortic wall of the thoracic aorta. The aortic wall is made up of 3 layers of tissue. When a tear occurs in the innermost layer of the aortic wall, blood is then channeled into the wall of the aorta separating the layers of tissues. This generates a weakening in the aortic wall with a potential for rupture. Aortic dissection can be a life-threatening emergency. The most commonly reported symptom of an acute aortic dissection is severe, constant chest or upper back pain, sometimes described as "ripping" or "tearing." The pain may move from one place to another.
When a diagnosis of aortic dissection is confirmed, immediate surgery or stenting is usually done.
What causes aortic dissection?
The cause of aortic dissection is unclear. However, there are several risk factors associated with aortic dissection, such as:
-
High blood pressure
-
Connective tissue disorders, such as Marfan disease, Ehlers-Danlos syndrome, and Turner syndrome
-
Cystic medial disease (a degenerative disease of the aortic wall)
-
Aortitis (inflammation of the aorta)
-
Atherosclerosis
-
Bicuspid aortic valve (only 2 flaps in the aortic valve, rather than the normal 3)
-
Trauma
-
Coarctation of the aorta (narrowing of the aorta)
-
Excess fluid or volume in the circulation (hypervolemia)
-
Polycystic kidney disease (a genetic disorder characterized by the growth of numerous cysts filled with fluid in the kidneys)