Clinical Training
Introduction

Fellows enter a three-year clinical and research program equipping them with a foundation in Pulmonary and Critical Care Medicine, and tools to launch a successful academic career. This includes 18 months of clinical / ambulatory care training as required by the Accreditation Council of Graduate Medical Education. There are eight contiguous inpatient rotations (the “clinical year”), outpatient clinics, and additional rotations during the 2 years otherwise devoted to research. Most Fellows devote an additional optional year to research or coursework leading to a Masters degree in Clinical Investigation. Rotations are described in the sections below.
Clinical Physiology at Johns Hopkins Hospital

The Physiology rotation provides each fellow the opportunity for closely guided, in-depth study of pulmonary and sleep physiology, akin to a college seminar course with a class of one. Under faculty supervision, the fellow:
- Supervises and interprets cardiopulmonary exercise testing
- Reads all pulmonary function testing at Johns Hopkins Hospital
- Performs and interprets special testing such as dead space and compliance measurement
- Meets with a faculty member 2-3 times weekly for one-on-one tutorials in pulmonary physiology, PFTs, and laboratory practice
- Completes extensive reading in cardiac and pulmonary physiology
- Learns management of a large pulmonary function laboratory
Consultation Service at Johns Hopkins Hospital
The Pulmonary Consultation Service team consists of a faculty attending, two fellows, residents, and students on elective rotations. Approximately 800 consultations and 600 bronchoscopies are requested yearly. The consult team is also responsible for the care of inpatients who are on the Pulmonary Service. Fellows learn the latest diagnostic and management approach to common and rare diseases, including:
- Interstitial lung diseases
- Obstructive lung diseases, including one of the largest adult cystic fibrosis cohorts in North America
- Infectious diseases of the lung
- Diseases of the immunocompromised host
- Vascular diseases
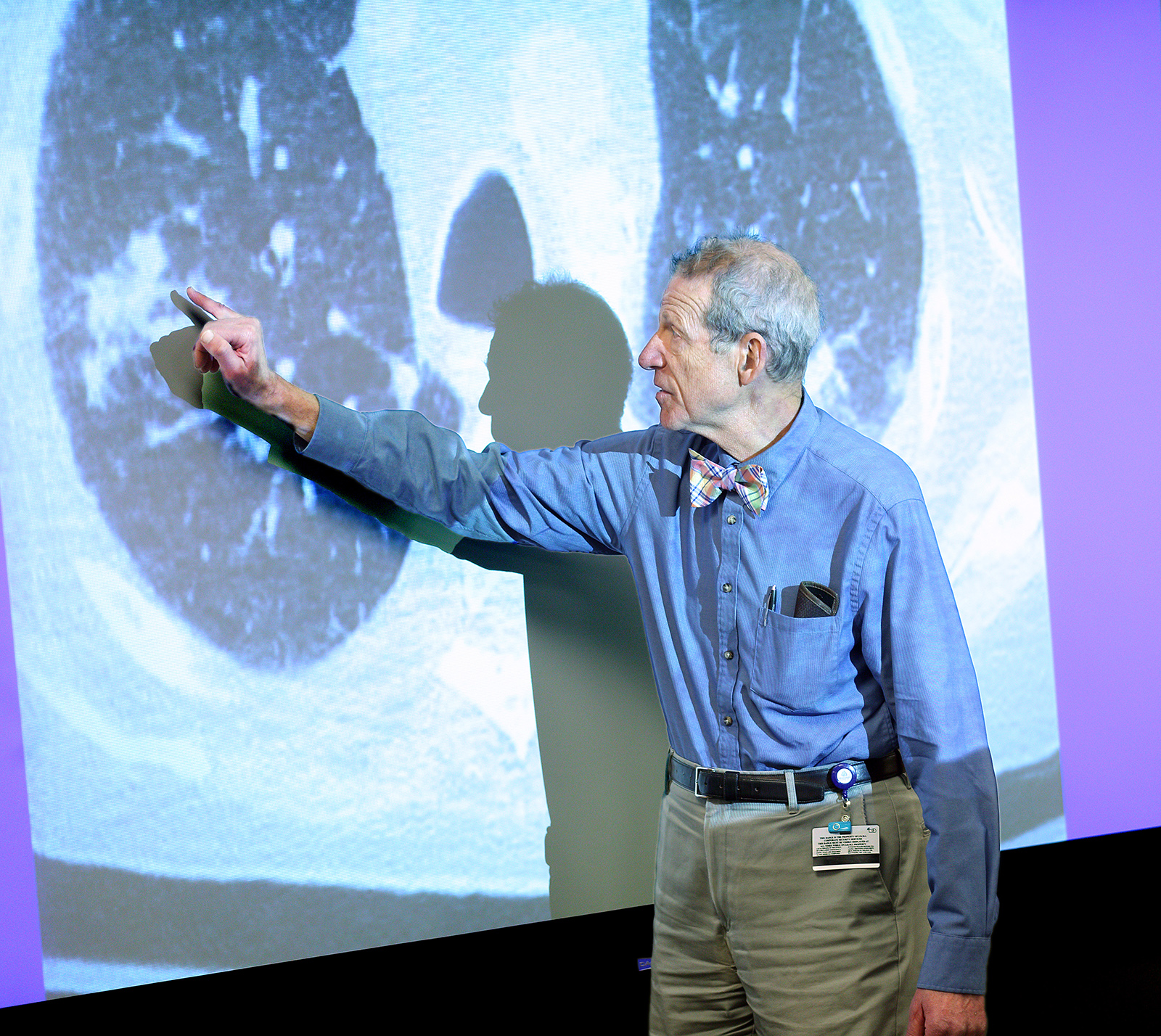
Fellows have extensive opportunities in bronchoscopy, and organize a weekly radiology teaching conference attended by Pulmonary and Radiology faculty.
Progressive Care/Consultation Service at Hopkins Bayview Medical Center

The Pulmonary Service team consists of a faculty attending, a fellow, and Nurse Practitioners and Physician Assistants. The attending and fellow supervise an active inpatient service of patients in the Progressive Care Unit and also provide approximately 200 pulmonary consultations and 150 bronchoscopies per year. The smaller size of this hospital encourages a close working relationship with house staff and attending physicians. Fellows function more as junior attendings in the supervision and delivery of pulmonary subspecialty inpatient care. Bayview consult Fellows have in-depth exposure to:
- Chronic Obstructive Lung Disease
- Difficult Asthma
- Geriatric care
- Multidisciplinary case management
Critical Care Service at Johns Hopkins Hospital

The MICU at the Johns Hopkins Hospital is a closed unit with 7-800 several hundred admissions per year. To better balance teaching with patient care service, the MICU is split into two teams, each including an attending, Fellow, residents, and subinterns. Fellows rotate through the MICU twice during fellowship. The Fellows make daily work/ teaching rounds and take turns with the attendings to give daily didactic sessions for the house staff. The attending and fellow also provide consultations on patients admitted to other critical care units. Fellows receive experience with:
- Mechanical and non-invasive ventilation
- Adjuvant therapy for respiratory failure (prone positioning, NO, etc.)
- Management of multisystem failure
- Management of end-stage solid organ transplant candidates
- Dialytic therapy
- Multidisciplinary patient management
- Medical ethics and end-of-life issues
- Health economics
- Unit organization, patient safety, and clinical management protocols
Critical Care Service at Hopkins Bayview Medical Center

The MICU at Hopkins Bayview Medical Center is a 12 bed closed unit with approximately 400 admissions per year. As at Hopkins Hospital, the MICU team includes a faculty attending, fellow, and dedicated MICU house officers. The duties of the fellow are similar to those in the MICU at Johns Hopkins Hospital, but the fellows are encouraged to assume a more active role as team leader. Special opportunities at the Bayview MICU include:
- Emphasis on ventilation and rehabilitation of obstructive lung disease, very common in the surrounding community
- Long-term weaning through the long term ventilation unit at the Bayview Geriatric Center next to the hospital
- Consultation on patients in the Burn Unit
Oncology Critical Care Service at Johns Hopkins Hospital

The Sidney Kimmel Comprehensive Cancer Center at Johns Hopkins Hospital was established in 1973. The Center has high-volume hematopoietic stem cell transplant, leukemia, and solid tumor programs. The Oncology Critical Care Service provides care for all critically ill patients in the cancer center in a closed 6-bed intensive care unit on Weinberg 5C. Typical patients have life-threatening complications of malignancies or treatments for malignancies, including acute leukemia, hematopoietic stem cell transplant, and complications of immunotherapy and CAR-T cell treatment. Typical diagnoses include acute respiratory failure, neutropenic sepsis and septic shock, seizures and encephalopathy, intracranial hemorrhage, acute liver failure and acute kidney failure. The critical care team consists of an attending faculty member from the Division of Pulmonary and Critical Care Medicine, a pulmonary and critical care fellow, and an experienced nurse practitioner or physician assistant. The attending and fellow are also responsible for providing consultative services on in- and out-patients in the cancer center with pulmonary infiltrates, masses, coin lesions, pneumonia, pleural effusions, etc. Fellows develop expertise in:
- Respiratory failure in immunocompromised hosts
- Septic shock in immunocompromised hosts
- Critical care and pulmonary issues in bone marrow transplant recipients
- Complications of acute leukemia
- Complications of immunotherapy and immune effector cell therapy, including checkpoint inhibitors and CAR-T Cells.
- Interdisciplinary management of complex patients
- Hands-on procedural training, including direct and video laryngoscopy, bronchoscopy, ultrasound-guided vascular access procedures, thoracentesis, and chest tube placement
- End-of-life prognostication and palliative care
Advanced Lung Disease Service at Johns Hopkins Hospital

The Fellow on Special Services manages a busy in-patient service of patients with pulmonary hypertension or lung transplants. Lung transplantation is a large multidisciplinary joint program with the Department of Surgery. Fellows participate in the pre-transplant evaluation, peri-operative care, and post-transplant management. The Division also cares for 500 patients with pulmonary hypertension, 100 of whom are receiving either approved or investigational agents as part of clinical trials. The pulmonary hypertension clinic sees about 200 new patients each year, most of whom undergo right heart catheterization and vasodilator trials. Fellows will learn:
- Work-up and treatment of pulmonary hypertension
- Transplant evaluation, indications, pre-operative management
- Immunosuppressive therapy
- Management of acute and chronic rejection
- Management of right heart failure
Second and Third Year Rotations
During the 2nd and 3rd year, Fellows complete block rotations totaling 3 months/year. These include interventional pulmonology, rotations in two Surgical Intensive Care Units, Anesthesiology, an Ambulatory Care Block during which they attend several of the subspecialty pulmonary clinics, and blocks of neurological/neurosurgical critical care and cardiovascular surgical critical care. These provide advanced training in procedural skills and experience in critical care in non-medical settings.
Outpatient Clinics

Approximately 6,000 patients are evaluated yearly (14,000 patient visits) in a variety of general and subspecialty clinics. Fellows staff a highly regarded Fellows teaching continuity clinic, and rotate through specialty clinics including:
- Cystic Fibrosis
- Sleep Disorders
- Sarcoidosis
- Interstitial Lung Disease
- Lung Transplantation
- Asthma
- COPD
- Neuromuscular Disease
- Lung Cancer
- Non-tuberculous mycobacteria and bronchiectasis
These specialty clinics give Fellows the opportunity to work with world-renown clinicians and researchers in specific disease areas. Fellows who elect their research experience in these areas generally also staff the associated clinic during their research years.
Conferences

The Division and Department of Medicine have more conferences than a Fellow could ever hope to attend. Conferences are attended by Fellows during their research and clinical years. Core conferences held weekly for or by the Fellows are:
- Fellows’ Journal Club
- Fellows’ Research-in-Progress
- Pulmonary Radiology Conference
- Pulmonary Grand Rounds
- PCCM Core Curriculum Lecture Series
- Lung Research Conference
Fellowship opens with a day-long hands-on course in bronchoscopy and other procedures in our Simulation Center. We have a Summer Lecture Series during July and August to rapidly bring new Fellows up to a level of comfort managing subspecialty patients and fielding questions from house staff. Other Pulmonary didactic teaching sessions include morning conferences in the Bayview and Hopkins Hospital MICU, a weekly multidisciplinary Critical Care journal club, MICU/SICU case conference, and an evening dinner/lecture series on essential skills for an academic career.
