Noninvasive Liquid Biopsies Rapidly, Accurately Determine Response to Cancer Treatment
02/13/2019
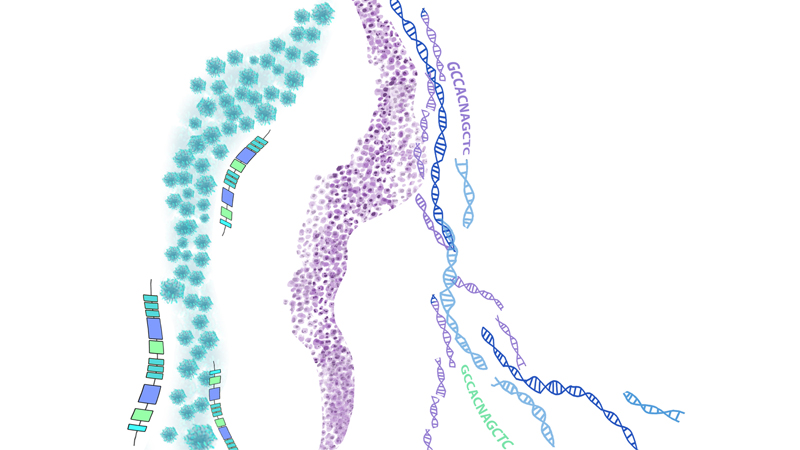
Results of two clinical studies have added to evidence that blood-based liquid biopsies can accurately track lung cancer treatment responses by measuring circulating tumor DNA (ctDNA) during immunotherapy and related treatments.
“There is an unmet clinical need for real-time, noninvasive detection of tumor response to targeted and immune checkpoint blockade treatments,” says Victor Velculescu, M.D., Ph.D., co-director of cancer biology at the Johns Hopkins Kimmel Cancer Center. “Our studies suggest that tests using blood samples will change the way cancer patients will be treated by helping to evaluate therapeutic responses more quickly and accurately, and avoid unneeded toxicity or ineffective treatments.”
In a study of 28 adult patients with advanced nonsmall cell lung cancer (NSCLC), blood samples were taken prior to anti-EGFR (epidermal growth factor receptor) or anti-HER2 (human epidermal growth receptor 2) treatments—which target cancer growth—and at intervals thereafter.
All of the patients were seen at hospitals affiliated with The Johns Hopkins University or University of California San Diego, and were treated with osimertinib, mavelertinib, afatinib or erlotinib. Blood samples were analyzed to detect ctDNA shed by tumors into circulating blood and to track tumor burden during therapy by detecting gene mutations as well as chromosomal changes in tumor cells.
As early as a week after receiving treatment, 16 patients with molecular response to treatment had nearly complete elimination of ctDNA that could be detected in their blood samples. Eight nonresponders to the therapy had limited changes in ctDNA levels and significantly shorter progression-free survival. Overall, patient response to treatment could be detected four weeks earlier and was more accurate than CT imaging.
The researchers also say that ctDNA analyses of patients with stable CTs or nonmeasurable disease using imaging had improved prediction of clinical outcomes compared to patients with CT imaging.
“These results indicate the potential value of early assessment of responses to targeted therapies especially when CT imaging results are in the gray area between objective response and actual disease progression,” says Alessandro Leal, M.D., a graduate student at the Kimmel Cancer Center.
The early detection of changes using ctDNA preceded responses seen in subsequent scans and allowed mutation changes in the tumors to be tracked. With these results, the study showed that measuring ctDNA for an advanced cancer can be accurate and noninvasive than with repeat CT imaging.
“Noninvasive liquid biopsies identifying tumor-specific changes provide an opportunity for widespread implementation of monitoring approaches for different cancer types in a variety of clinical settings,” says Jillian Phallen, Ph.D., postdoctoral fellow at the Kimmel Cancer Center.
In a second study of 38 patients with NSCLC, scientists including Valsamo Anagnostou, M.D., Ph.D., assistant professor of oncology at the Johns Hopkins University School of Medicine and a member of the Kimmel Cancer Center, measured ctDNA and immune blood cell changes to determine responses to anti-PD-1 therapy, which boosts the immune response against cancer cells.
Nine patients with a clinical response to immunotherapy had a complete reduction in ctDNA levels shortly after the initiation of therapy. In contrast, 10 nonresponders showed no significant changes or increase in ctDNA levels. Molecular response, as measured by ctDNA levels, more accurately predicted overall survival for these patients—patients without a molecular response had shorter progression-free and overall survival than molecular responders. Overall, tumor responses to the therapy that were detected using ctDNA were found nearly nine weeks earlier than with conventional imaging.
Anagnostou and colleagues also investigated changes in the immune cells in the blood of these patients. Expansion of immune cells mirrored the ctDNA reduction during therapeutic response, suggesting that ctDNA reduction in circulating blood was in line with an effective immune response.
Anagnostou says the researchers also validated their findings in a group of early stage NSCLC patients who received anti-PD1 therapy prior to removal of their tumors. The researchers found that ctDNA molecular responses accurately captured the effect of immunotherapy. The authors also showed that reduction in tumor size after immunotherapy correlated with reductions in ctDNA levels.
“Conventional imaging does not always or quickly capture the unique timing and pattern of response to immunotherapy, highlighting the urgent need to develop biomarker-driven approaches such as measuring ctDNA in blood samples,” Anagnostou says. “Early detection of disease progression on immunotherapy opens a window of opportunity in which changes in liquid biopsies may allow patients with resistance to be rapidly identified and redirected to receive alternative therapies.”
Together, these studies show that noninvasive liquid biopsy analyses of ctDNA changes during therapy are feasible and offer a more rapid and accurate assessment of treatment response than CT imaging. Velculescu cautions that more testing will be necessary to affirm the value of the results and to see if this method works for other types of cancer. He says he hopes the studies will spur development of new therapies by being able to diagnostically measure tumor loads more accurately.
For the targeted therapy study, authors besides Velculescu and Leal are Anagnostou, Phallen, Brian Woodward, Patrick Forde, Jarushka Naidoo, Kristen Marrone, Julie Brahmer, Jacob Fiksel, Jamie Medina, Stephen Cristiano, Doreen Palsgrove, Chris Gocke, Daniel Bruhm, Parissa Keshavarzian, Vilmos Adleff, Elizabeth Weihe, Robert Scharpf and Hatim Husain.
For the checkpoint blockage study, authors other than Velculescu and Anagnostou are Forde, Naidoo, Marrone, Bruhm, Phallen, Leal, Adleff, Brahmer, James White, Noushin Niknafs, Carolyn Hruban, I.K. Ashok Sivakumar, Kellie Smith, Tricia Cottrell, Lamia Rhymee, Doreen Palsgrove, Christine Hann, Benjamin Levy, Josephine Feliciano, Christos Georgiades, Franco Verde, Peter Illei, Qing Kay Li, Edward Gabrielson, Malcolm Brock, James Isbell, Jennifer Sauter, Janis Taube, Robert Scharpf, Rachel Karchin, Drew Pardoll, Jamie Chaft and Matthew Hellmann.
COI:
Phallen et al. manuscript:
Forde has been a consultant for AstraZeneca/MedImmune and Boehringer Ingelheim. Adleff is a consultant for Personal Genome Diagnostics (PGDx). Velculescu is a founder of, holds equity in, and is a board of directors member at PGDx. Under a license agreement between PGDx and The Johns Hopkins University, Velculescu is entitled to a share of royalty that the university receives on sales of services or products by PGDx. Velculescu is a member of Ignyta’s scientific advisory board. The Johns Hopkins University has reviewed and approved the terms of these arrangements in accordance with its conflict of interest policies.
Anagnostou et al. manuscript:
Forde receives research funding for clinical trials from Bristol-Myers Squibb, AstraZeneca/MedImmune, Kyowa, Corvus and Novartis, and is a consultant/advisory board member for AbbVie, AstraZeneca, Bristol-Meyers Squibb, Boehringer Ingelheim, Celgene, EMD Serono, Inivata, Lilly, Merck and Novartis. White is a consultant for Personal Genome Diagnostics. Naidoo receives research funding from Merck, AstraZeneca/MedImmune, Kyowa and Calithera, and is a consultant/advisory board member for Bristol-Myers Squibb, AstraZeneca/MedImmune and Takeda. Hann is a consultant/advisory board member for AbbVie, Bristol-Myers Squibb and Genentech, and she receives research funding from Merrimack Pharmaceuticals, GlaxoSmithKline, AbbVie and Bristol-Myers Squibb. Taube is an advisory board member for Bristol-Meyers Squibb, Merck, AstraZeneca and Amgen, and she receives research funding from Bristol-Meyers Squibb. Levy is a consultant/advisory board member for AstraZeneca, Celgene, Genentech Rouche, Eli Lilly and Takeda, and he receives research funding from Celgene and Boehringer Ingelheim. Brahmer receives research grants from Bristol-Myers Squibb, AstraZeneca/MedImmune and Merck, and she is a consultant/advisory board member for Bristol-Myers Squibb, AstraZeneca/MedImmune and Merck. Brock is a paid consultant for Cepheid. Pardoll receives research support from Bristol-Myers Squibb, Compugen and Potenza Therapeutics, and he is a consultant for Aduro Biotech, Amgen, AstraZeneca/MedImmune, Bayer, Compugen, DNAtrix, Five Prime, GlaxoSmithKline, ImmuneXcite, Jounce Therapeutics, NexImmune, Pfizer, Rock Springs Capital, Sanofi and Vesuvius/Tizona. Velculescu is a founder of, holds equity in, and is a board of directors member for Personal Genome Diagnostics (PGDx). Under a license agreement between PGDx and The Johns Hopkins University, Velculescu is entitled to a share of royalty that the university receives on sales of services or products by PGDx. Velculescu is a member of the Ignyta scientific advisory board.
