Research Story Tip: International Johns Hopkins Study Says Broad Measures Needed to Prevent TB Spread in India
08/04/2020
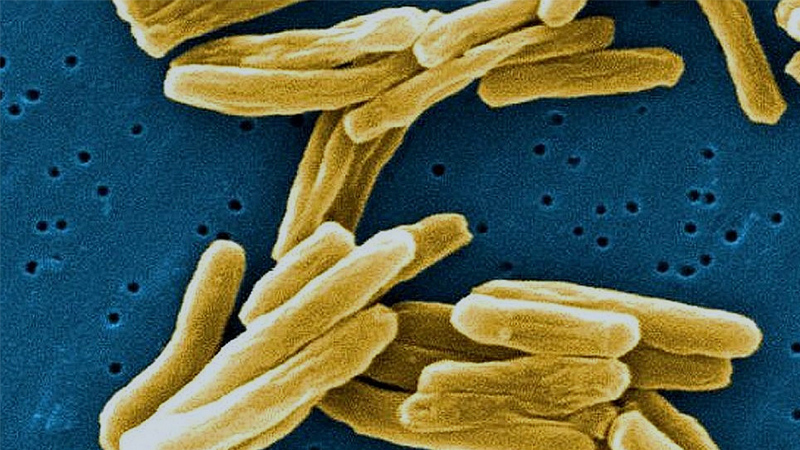
While tuberculosis, or TB, may not be a major health problem in the United States, the World Health Organization (WHO) reports it is still the leading cause of death worldwide from a single infectious agent (the microbe Mycobacterium tuberculosis) and is responsible for some 1.5 million fatalities annually. TB is especially serious in India, the country that accounts for 27% of all global cases of the disease.
Recently, the WHO changed its guidance for preventive treatment in countries with a high TB prevalence, recommending proactive drug therapy for all members of households exposed to TB by someone in the home with the pulmonary form of the disease. This is a departure from the current national guidelines in India that only require preventive TB therapy for children under age 6 and people living with the human immunodeficiency virus (HIV).
However, the new WHO recommendations for broader preventive measures is conditional and not based on strong evidence, so health officials in countries such as India wanted more proof that a switch in policy was warranted. Thanks to a new research study led by Johns Hopkins Medicine in collaboration with two Indian medical institutions, science and statistics are now backing the move.
The C-TRIUMPH (Cohort for TB Research with Indo-US Medical Partnership) study, which was reported in the July 29, 2020, issue of the journal PLOS One, was conducted under the Regional Prospective Observational Research in Tuberculosis Consortium for India (RePORT India), a consortium of coordinated TB research efforts across India funded by the governments of India and the United States. RePORT India is part of RePORT International, a larger collaborative undertaking similar work in five other high-burden TB nations: Brazil, China, Indonesia, the Philippines and South Africa.
The collaborating institutions on the study in India are the BJ Government Medical College (BJGMC) in Pune and the National Institute of Research in TB (NIRT) in Chennai.
The research team that conducted the study in India was directed by Amita Gupta, M.D., professor of medicine at the Johns Hopkins University School of Medicine. The data analysis was led by Mandar Paradkar, M.B.B.S., D.C.H., M.P.H., study coordinator at the BJGMC Clinical Research Site in Pune, in coordination with U.S. senior author Robert Bollinger, M.D., the Raj and Kamla Gupta Professor of Infectious Diseases and professor of medicine at the Johns Hopkins University School of Medicine.
For their study, the researchers in India enrolled 1,051 adults in the cities of Pune and Chennai who had been exposed to someone in their household with pulmonary TB. The 997 participants who completed the study were screened for both TB infection (presence of the bacteria) and TB disease using clinical, microbiologic and radiologic methods at enrollment, at sometime between four and six months, and at 12 and 24 months.
“We found that 707 of the 997 participants, or 71%, tested positive for TB infection at the start, and 20, or 2%, subsequently developed the disease during 24-month follow-up period,” says Paradkar. “Based on these numbers, we estimate that that 12 people per 1,000 per year will get TB disease through a household contact. This is a large enough rate to support the new WHO guidelines for stopping the spread of the bacteria, calling for all residents in households with TB present to receive therapy without needing to first be tested for infection.”
Paradkar adds that the development of TB disease through household exposure was not associated with smoking, alcohol consumption, diabetes mellitus or when TB infection was detected during the study period.
To increase the effectiveness of TB prevention on a large scale, the new WHO recommendations provide options for shorter-duration treatments in addition to the previous course of the antibiotic isoniazid daily for six months. The alternatives include: one month daily regimen of another antibiotic, rifapentine, plus isoniazid; three months weekly rifapentine plus isoniazid; three months daily rifampicin plus isoniazid; or four months of daily rifampicin alone.
“The findings from our study will help inform national protocols for the screening of household contacts of TB patients and the administration of appropriate preventive therapy in India and other high-burden TB regions of the world,” says Bollinger.
