Milestones in Radiation Oncology
Excellence in proton therapy emanates from excellence in all areas of radiation oncology. Our National Proton Center is built upon a strong history of breakthrough discoveries and scientific ingenuity.

Johns Hopkins is among the first to be designated a Comprehensive Cancer Center by the National Cancer Institute. Medical oncologists, radiation oncologists, surgeons, oncology nurses, researchers and other specialists work together to advance cancer treatment and research.
Radiation oncology broke off from the Department of Radiology and Radiological Sciences and joined forces with the Department of Oncology to make progress against a growing cancer epidemic.
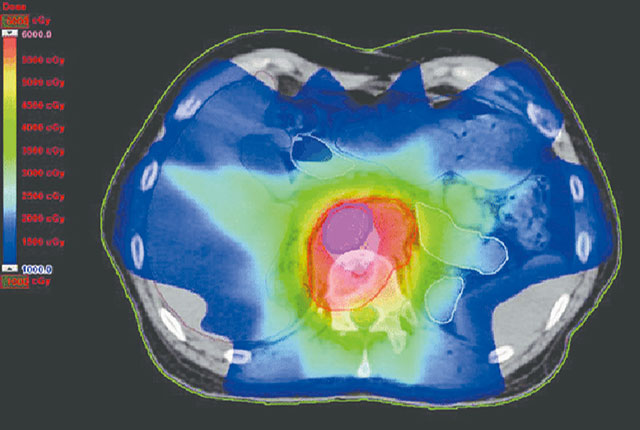
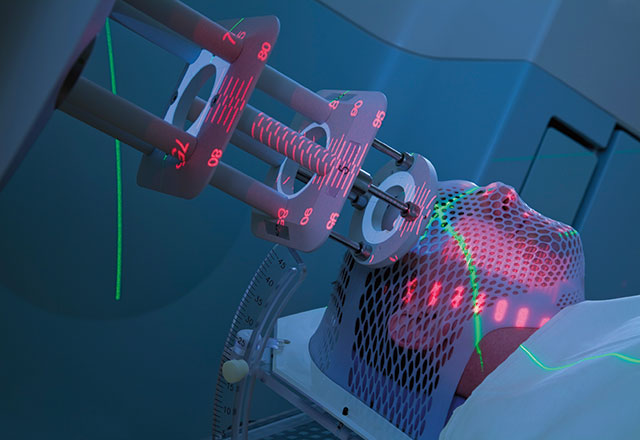
The Intensity Modulated Radiation Therapy Program began to deliver high-precision radiation that conforms to the three-dimensional shapes of tumors and delivers higher and well-defined doses of radiation to tumors, and even specific areas within tumors, while minimizing radiation to surrounding normal tissue.
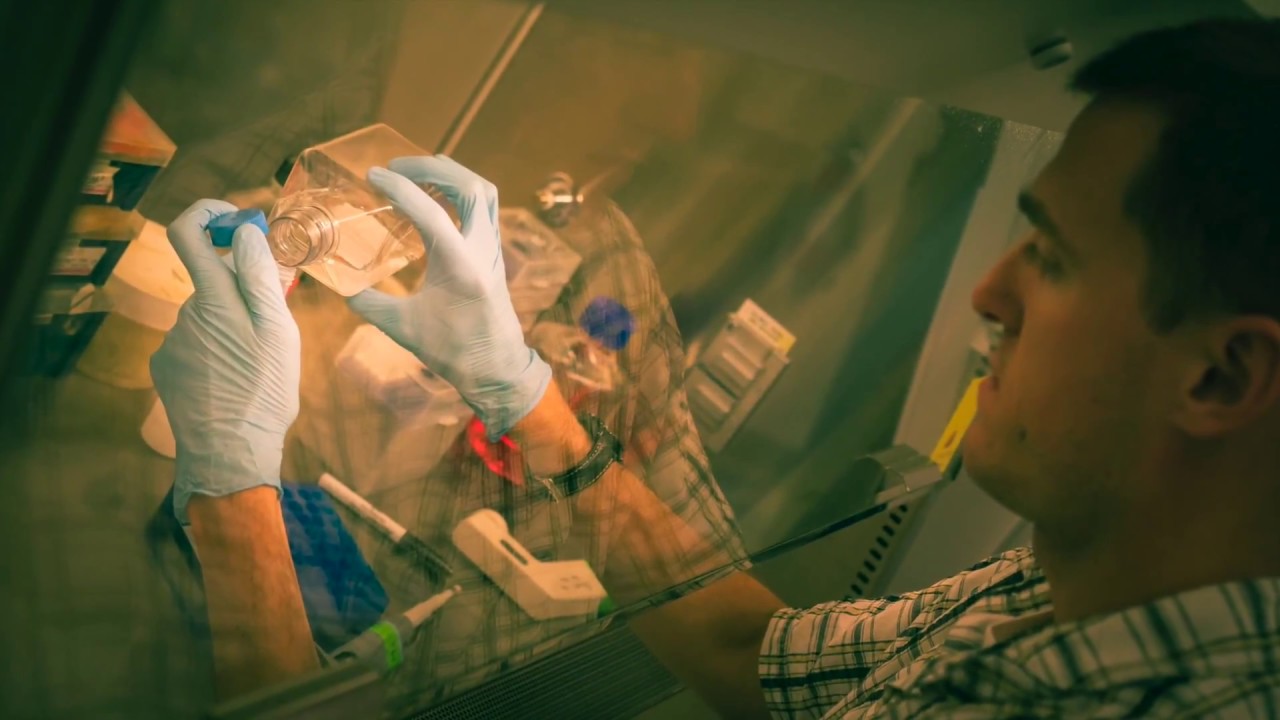
Research reveals that lower doses of radiation may kill more cancer cells byeluding a protein called ATM, a damage detection mechanism for cancer cells.
Science Watch newsletter dubs the Kimmel Cancer Center a “cancer research powerhouse,” as its research is the most often cited in all of cancer research worldwide.
Molecular Radiation Sciences research accelerated to decipher the biology of DNA damage response to radiation therapy and how cells sense and repair this damage.
Research showed that men whose tumors recurred after prostate cancer surgery are three times more likely to survive their disease long term if they underwent radiation therapy within two years of the recurrence.
A computer-assisted version of brachytherapy, a prostate cancer therapy that uses radioactive seeds inserted in the prostate to kill cancer cells, is developed. The innovation allows for more precise placement of seeds. An even more precise version followed, using an MRI-assisted robotic needle to accurately insert the seeds.

A unique collaboration between our Department of Radiation Oncology at Sibley and Children’s National pediatric cancer center results in the first dedicated pediatric radiation oncology program in the national capital region. It brings together pediatric medical and surgical oncology experts from Children’s National and pediatric radiation oncology experts from the Kimmel Cancer Center to provide comprehensive pediatric cancer care, including clinical trials, to patients in the region.
Stereotactic radiotherapy is shown to augment immune response in pancreatic cancer patients.
The Kimmel Cancer Center at Sibley Memorial Hospital opens adding medical oncology and surgical oncology to the already established and growing radiation oncology program. The 36,000-square-foot facility brings patients the most advanced radiation therapy technologies, latest techniques and innovative treatments—the same techniques and technologies used throughout the Johns Hopkins Kimmel Cancer Center.