ALTHOUGH JOHNS HOPKINS Medicine has made notable
strides on the institution’s patient- and family-centered care
strategic priority, December’s Town Meeting focused on
the work that lies ahead. In his opening remarks, Ronald
R. Peterson, president of the Johns Hopkins Health System
and executive vice president of Johns Hopkins Medicine,
outlined impressive gains in delivering care that is “compassionate,
respectful and personalized.” Renovated facilities, a
stronger command of diagnostic tools, the updated Patient
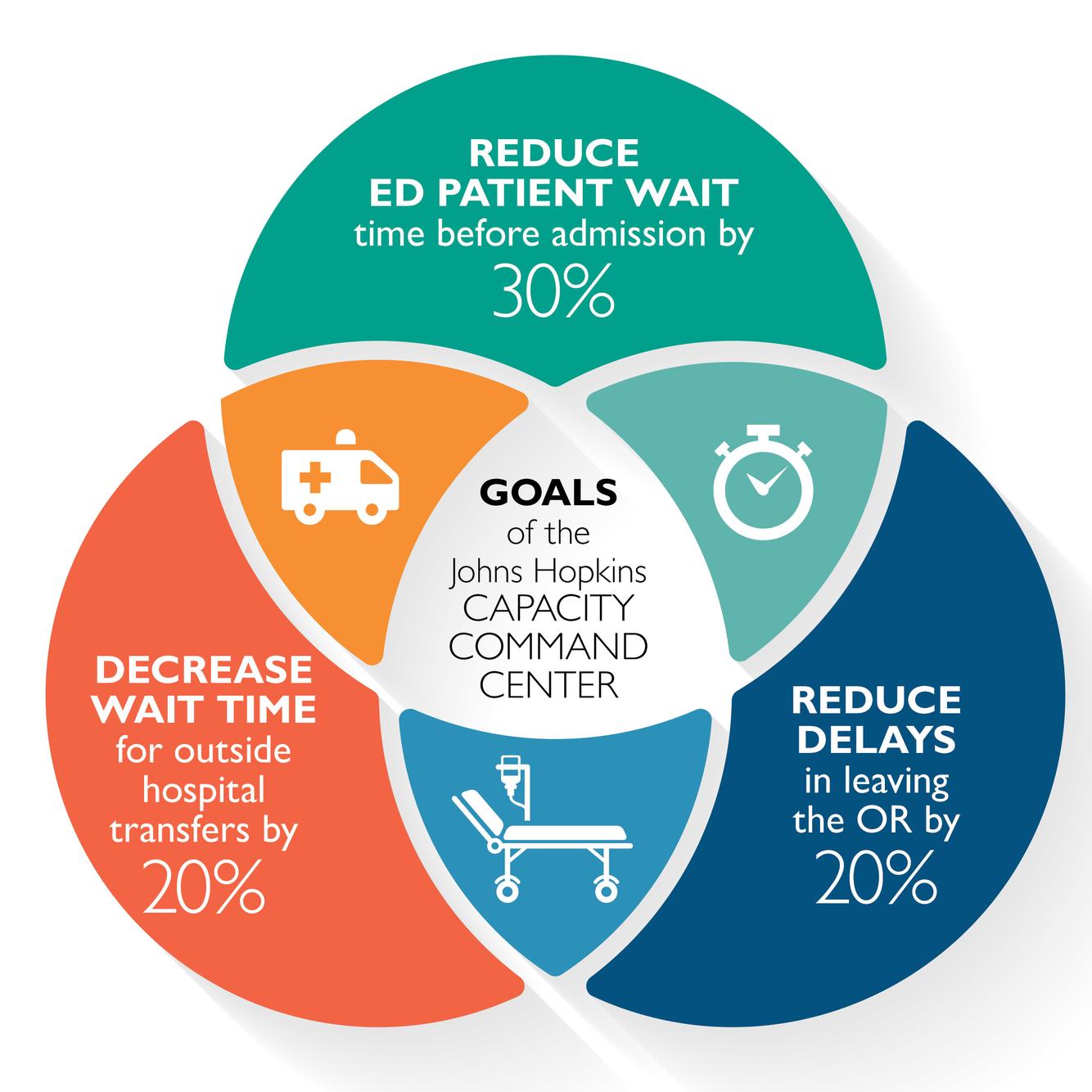
and Family Handbook, and the Judy Reitz Capacity Command
Center have all furthered the institution’s strategic
goals, Peterson said.
During the panel discussion that followed, participants also acknowledged the need for improvement across the care continuum. “Today and in ongoing conversations, it’s important to speak up and to discuss anything you think that does not feel right,” said panel moderator Deborah Baker, senior vice president for nursing for the Johns Hopkins Health System. A more forthright and cohesive workforce is essential to better care, Baker said. “The empathy we build with each other helps us to treat patients better.”
Panelist Richard Dean, a member of the Johns Hopkins Hospital oncology unit’s Patient and Family Advisory Council, praised the care his wife and daughter received as cancer patients and noted gaps as well. “I have a different set of eyes and can bring ground truths to the reality of what it’s like to be a patient in the Johns Hopkins system.”
Improving the patient experience often boils down to improving communication, said panelist Lisa Cooper, vice president of health care equity for Johns Hopkins Medicine. “There is a science of patient-centeredness,” she said. When “patients get clear communication with health care professionals, they’re more likely to follow through on prescriptions, know what’s expected of them and come back.”
Care that is patient- and family-centered must establish health care equity, Cooper said. Focusing on each patient as an individual may cause caregivers to overlook health disparities among populations “who consistently have poor experiences in our health care systems,” including ethnic minorities, those who live in poverty, members of the LBGT community and people with disabilities.
As Johns Hopkins embraces precision medicine directed to each individual’s genetic and biological makeup, Cooper cautioned practitioners to keep in mind the social and cultural circumstances that contribute to chronic health disparities. “We want to approach people as individuals,” Cooper said. But, she added, Johns Hopkins must also be thinking about groups of people with disadvantages that “we’re consistently overlooking.”
Other panelists included Lisa Allen, chief patient experience officer for Johns Hopkins Medicine, and Holley Farley, a nurse clinician with the hospitalist unit.