As the pandemic surged in 2020, the Emergency Department quickly became the epicenter for patients with COVID-19 entering the hospital. HCGH ED nurses found their roles and responsibilities in a constant state of flux as the word “pivot” took on new meaning. Their processes and workflow were continually being redefined as the pandemic bore down on the ED.
Jen Ayd, RN, joined the HCGH ED staff in April 2020, in the thick of the pandemic. While 2020 presented many challenges to ED nurses, for Jen, it also brought many bright moments that have forever changed her as a nurse.
“The biggest change we saw immediately was absorbing so many roles and responsibilities that were never ours before. That list is a mile long.
“With family members not permitted to be at their loved one’s side, we are more connected and have become that bridge between them and the patient. Families feel helpless – it is scary sending their loved one into the ED and then having to wait in the car. When I walk outside the ER at night, everyone has their car dome lights on and it hits you that it is a waiting room out there. I look at them and see cars occupied with worried family members. There's nowhere for them to go, and they don't want to leave, even though there's not much that they can really do.
“This has really impacted me and made me change the way I communicate with families. Before COVID, so much of the communication was between the patient and their family member. Now that communication is often between the nurse and the family member. You can just hear the stress and worry leave the voice of the family member when they feel confident that you're taking good care of their loved one. That open line of communication makes a huge impact and is something I would want if my family was in the hospital.“We took on the responsibilities of patient transport, and for the better part of a year, we spent a lot of our time in PPE standing in the hallway waiting for our patients to come out of imaging.
“Our workflow has also seen a dramatic shift. Where we once could come and go out of a patient’s room as needed, we now try and “cluster care,” to minimize multiple interactions with the patient, to reduce potential spread. It's definitely a challenge. You don't have the ability to just leave and get supplies. Early in the pandemic, you had to be constantly aware of your surroundings and extra prepared before you enter a patient room. It kind of takes away your independence, and you have to rely on other nurses more than you ever have. You also constantly had to have a bigger view of the unit because at any given point there could likely be a coworker on the other side of a glass door trying to get your attention.
“We have continued to refine our workflow process, and when a patient with COVID-19 comes in now, we have a primary nurse who goes right in and assesses the patient and a designated person who is always at their beck and call outside the room.
“As a nurse, it makes you realize that we're all in this together. It truly is team nursing. We've always been a team, but now it's different. You need your fellow nurses, and you cannot function without them.”
The ER in the Pandemic: A Nurse’s Story
Filling the Gaps and Being the Bridge
Related Reading
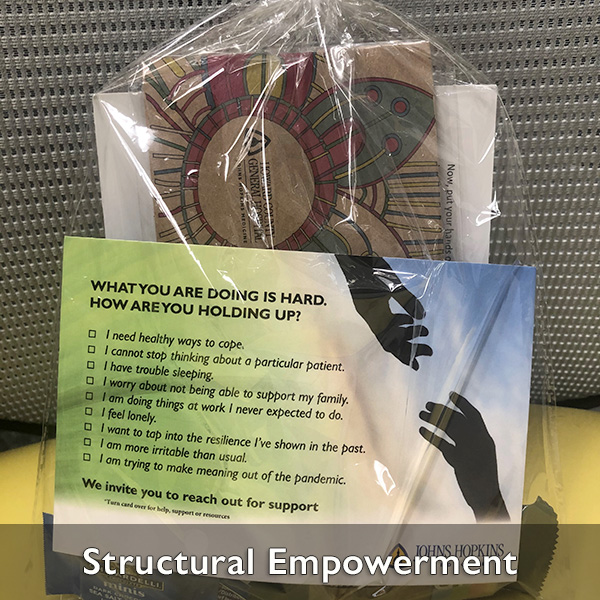
Collaborating to Support Resiliency
As the pandemic hit HCGH, it became critical to address the needs of nurses and clinical staff serving on the frontlines. A multi-department initiative was launched to support the staff’s greatest challenge – the need to stay resilient.