It was late in the day on Friday, February 28, 2020, when HCGH Chief of Infectious Disease Mark Landrum, M.D., and the infectious disease manager walked into the office of Clinical Education Program Manager Roslyn Katz, MSN, RN, CEN.
Roslyn recalls the conversation vividly, “Dr. Landrum told me we needed to start educating our staff on personal protective equipment (PPE). We had a big mandatory training event already planned and scheduled in two weeks with the Johns Hopkins Biomed Unit. I asked him if we could wait until then. His answer was, ‘No, we have to start right away.’ We knew this was going to be a massive undertaking, so we brainstormed together, initially coming up with the idea to use our scheduled huddles to demonstrate and educate the Emergency Department staff on how to properly don and doff PPE. I will never forget that day.”
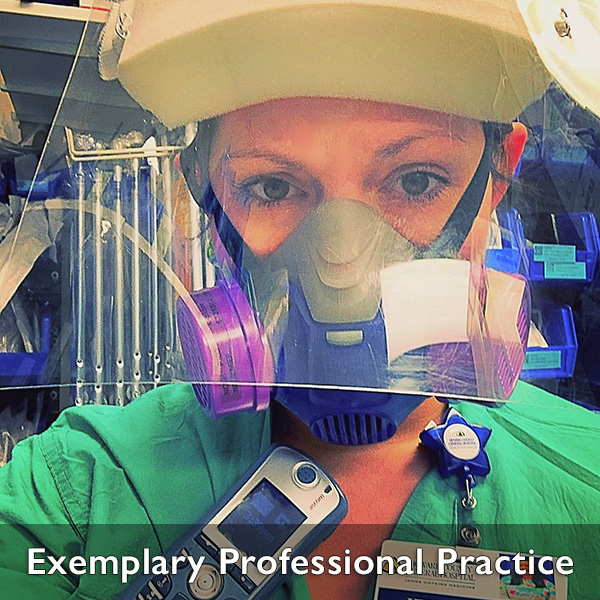
The start of the pandemic mostly focused on PPE training. Together with other hospital Clinical Education managers, the education team spent the next week creating educational plans and materials. A step-by-step instructional sheet was developed to help educate staff on the ‘buddy system’ and donning and doffing PPE. “We then started training other staff from clinical and nonclinical departments throughout the hospital,” says Roslyn. “I did a lot of discussion at the end of the classes about why we were doing this, why it's so important and how important it was to take care of ourselves so that we could take care of the patients and take care of each other. I feel like I did one month nonstop of PPE education training.”
Nurse education then turned to addressing challenges they knew were coming. These challenges included training non-critical care nurses to care for critically ill patients who were intubated, and safely care for patients with COVID-19. They also needed to identify which rooms were for COVID patients and who was permitted in the rooms. “Our team of nurse educators worked collaboratively with hospital physicians to make sure that we were all doing the right things based on evidence, and we created standards of care,” Roslyn says.
HCGH Clinical Education Program Manager Kim McKnight, MSN, RN, PCCN, CCRN-K, SCRN, CDP, realized the nurses on the hospital’s 3P Cardiac Unit and Observation Unit needed to train to care for critically ill patients, as the hospital shifted department functions to accommodate the anticipated influx of patients with COVID-19.
Kim recalls, “Our ICU became a COVID unit, and our step-down Special Care Unit (SCU) became the non-COVID ICU. So, we began preparing to have SCU patients on our two units. The nurses needed training on specific skills to prepare for that change. The ICU Clinical Education program Manager Catherine Miller, MSN, APRN-CNS, ACNS-BC, CCRN-K, and I ran a training we called ‘Critical Care Class for the Non-Critical Care Nurse,’ and we educated nearly 80 nurses between the two units.” This was a blended-learning curriculum. Prior to class, the nurses completed electronic learning modules, and the class included skill instructions at seven interactive stations using appropriate equipment.
The Cardiac Rehab Gym space was closed to patients early in the pandemic, and the educators collaborated to use the space and convert it to a teaching space, with demonstrations and hands-on skills stations, complete with a mannequin and ventilator. Stations included management of patients on a ventilator, post-cardiac catheterization management, invasive monitoring (such as an arterial line), titration of cardiac drips and insulin infusions.
Catherine says, “I was really encouraged by the nurses’ enthusiasm to learn these skills. They were very appreciative of the hands-on stations we set up for them, and to actually see that the ventilator is not as scary of a machine as they thought. They learned how to suction a patient, and how to manage the endotracheal tube, and how the respiratory therapist is our best friend in these situations.” Following the training, several of the nurses were deployed to the non-COVID ICU to care for critically ill patients.
“We recognized that we were asking the nurses to take on a lot of responsibility, so we wanted to make sure they realized that they were not on an island and they had the support that they needed,” Kim says. “I'm so proud of them all—they stepped up, were willing to learn and they were willing to work as a team.”