On a recent Saturday morning, Mark Rodgers is conversing with a group in the social hall of Garden of Prayer Christian Church in Waverly. The deacon is wearing a blue T-shirt that proclaims “Power to Stop Diabetes.” He says he’s determined to claim the title with support of a yearlong prevention program managed by Johns Hopkins.
Rodgers knows too well the disease’s deadly toll: he’s lost his father, grandmother, grandfather and several aunts to its complications. Last October, Melvin Tuggle, pastor of Garden of Prayer, also died from the disease.
“I’m changing my eating habits and trying to be more physically active, even though my schedule doesn’t really permit it,” says Rodgers, who works two jobs. “The last thing I feel like doing is cooking when I get home, but I’ve changed the food that I order when I order out.”
The Diabetes Prevention Program (DPP) — a partnership between the church and the Johns Hopkins Brancati Center for the Advancement of Community Care — is teaching Rodgers and six other participants at risk for type 2 diabetes about healthy eating and exercise. Their goal: reduce their diabetes risk by losing 5% of their weight and by exercising 150 minutes each week. The Brancati Center has trained two health coaches, who are also members of the church community, to help the group achieve success.
Type 2 diabetes, which is preventable, accounts for 90%–95% percent of national diabetes cases, according to the Centers for Disease Control and Prevention. This diabetes prevention model, which Johns Hopkins helped pioneer, proves that lifestyle changes can reduce participants’ risk perhaps even more than preventive medication. The Diabetes Prevention Program randomized trial, initially published in 2002, set the stage for the National Diabetes Prevention Program, which was established by the CDC in 2010.
“It was a very big deal to find that lifestyle change had such a big impact on diabetes risk reduction,” says Megan Brown, the Brancati Center’s program director.
The Brancati Center received full CDC recognition for its DPP in 2017 after participants in its first two programs exceeded CDC goals. In Maryland, this program is covered by both Medicare and Medicaid.
So far, 12 churches, schools and federally qualified health care centers have offered the program in partnership with the Brancati Center. Roughly 150 Marylanders, mostly in Baltimore, have participated, including 44 people who are currently enrolled.
At the recent gathering at the Garden of Prayer Church, the subject is the slippery slope of lifestyle change. Participants discuss their victories — one group member cut out fast food and soda — and their shortfalls, such as eating too much cake at a family get-together.
“They want to change their lifestyle. They don’t want to take medication to do it,” says Asha Hale, one of the Johns Hopkins-trained coaches and a lifelong member of the church. “This gives me an opportunity to help people in a way I didn’t think I could, especially people close to me. They’ve all known me since I was a baby.”
Less than halfway through the 12-month program, three people have already met their weight loss targets, and two more are close. They talk about keeping diaries of what they eat and trying new, healthy foods. When one participant says he struggles to go to the gym, another group member, Delores Murphy Powell, invites him to come to hers.
“We’re a close-knit church anyway, but this has caused my relationship with some of these people to become more intimate,” she says. “We support each other and chastise each other. We’re each other’s buddies through this whole thing.”Diabetes Prevention Program in Baltimore communities | Johns Hopkins Medicine Research
Johns Hopkins Medicine researchers engage in a diabetes prevention program for local Baltimore communities. Nisa Maruthur, M.D., M.H.S., a faculty member from The Brancati Center for the Advancement of Community Care shared why and how they worked as one site of the National Diabetes Prevention Program in Baltimore. Their recent study reports that few American adults eligible for diabetes prevention programs are being referred to, or participating in, these programs. Maruthur shares some suggestions for addressing the problem.
Meeting Community Needs
Established in 2015 to improve community health in partnership with community organizations, The Brancati Center was named for the late Dr. Frederick Brancati, a diabetes researcher who served as director of the Johns Hopkins Division of General Internal Medicine before he died in 2013 from amyotrophic lateral sclerosis (ALS).
The center performs community health screenings; supports research that aims to improve patient outcomes, lower costs and reduce health disparities; and supports educational activities that promote diversity in the health care workforce and offer opportunities for community education in East Baltimore. Initially funded by a gift from Walgreens in honor of Dr. Brancati, its programs are now funded by a variety of grants.
The center has broadened its programs to address HIV, substance abuse and nutrition.
“We focus on taking evidence-based interventions into the community,” says Nisa Maruthur, the center’s community partnership director and an associate professor of medicine, epidemiology and nursing at the Johns Hopkins University School of Medicine. “We don’t go there and tell people how to do things, they tell us how we need to do things. We take the science, take their perspective and put that together.”
That modus operandi is what’s guiding the center’s new program for people who already have diabetes. The diabetes self-management program developed by diabetes researcher Felicia Hill-Briggs, called Decision-Making Education for Choice in Diabetes Everyday (DECIDE), has been shown to reduce hemoglobin A1C, a measure of blood sugar, while also improving blood pressure and cholesterol levels.
“The program provides important knowledge and skills to help people take care of their diabetes each day in the context of the stress and responsibilities in their lives,” said Raquel Greer, an assistant professor of medicine and epidemiology at the Johns Hopkins University School of Medicine and the center’s education director. “We teach them problem-solving skills — how to identify the problems that get in the way of checking their blood sugar, taking their medications or eating a healthy diet each day, and how to identify and choose solutions that will work for them and lead to better health.”
Funded by the Johns Hopkins Urban Health Institute, the self-management program is currently underway at Zion Baptist Church in East Baltimore’s Oliver neighborhood. The Brancati Center plans to launch its second cohort at the church in January.
Filling a Gap
Maruthur, a general internist, was a medical student when the initial DPP study sparked her interest in diabetes prevention.
“There’s a huge burden of diabetes in our community,” she says. “People in Baltimore, especially in the neighborhoods we’re working in, are more likely to develop diabetes, need dialysis, have kidney failure from diabetes, develop blindness or need an amputation than those living in higher income areas. These things touch the lives of the participants that we see.”
The causes are complex: Low income areas have higher rates of diabetes, and residents with diabetes are more likely than those without the disease to live at least 15 minutes away from a grocery store, according to the 2014 Baltimore Community Health Survey. For those enrolled in DPPs, the high cost of healthy foods, lack of transportation and lack of access to places for physical activity can hinder success.
Melva Jones, a nursing coordinator for the Department of Psychiatry and Behavioral Sciences, served as a DPP coach trained by the Brancati Center in 2016. She says the program fosters camaraderie.
“To this day, people will come up to me and say, ‘I’m still eating healthy, I’m still maintaining my weight and I’m still logging my food because I see the benefit,’” Jones says. “Being a nurse, I see people all the time who have symptoms of diabetes and don’t realize what the symptoms mean.”
Symptoms of type 2 diabetes include frequent urination, thirst, fatigue and blurry vision, although those with prediabetes might not exhibit these signs. Risk factors for prediabetes include being overweight, being 45 or older, having an immediate family member with type 2 diabetes, being physically active less than three times a week, having had gestational diabetes or giving birth to a baby who weighed more than 9 pounds, and having polycystic ovary syndrome.
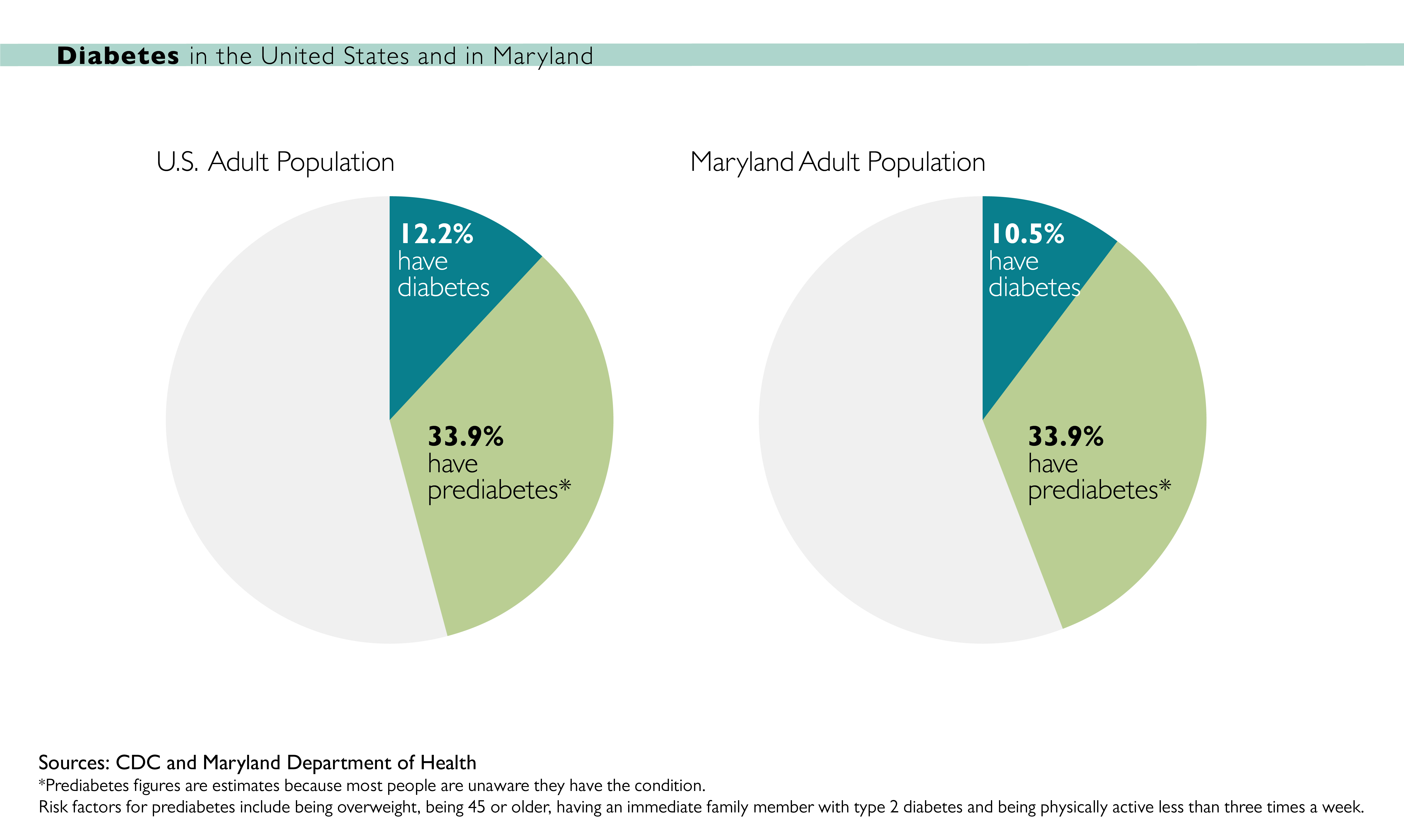
According to the CDC, an estimated 84.1 million American adults have prediabetes — more than 1 in 3 — but only 11.6% of them are aware of their condition. Of those who do know, few participate in, or are referred to, a diabetes prevention program, according to a study in the American Journal of Preventive Medicine by Brancati Center faculty member Maya Venkataramani, an assistant professor at the Johns Hopkins University School of Medicine.
“There’s a gap that we want to fill,” Maruthur says. “We’re developing a model for how to do DPPs and DECIDE so that we can transport the [Brancati Center model] to communities outside of Baltimore. We want to make sure that this is happening elsewhere.”
Johns Hopkins leadership is helping fund the effort. The Strategic Planning Executive Commission has committed to supporting the DPP for the next five years as the Brancati Center sets up its government reimbursement process. Maruthur is also working with her colleagues to establish a new clinical pathway across Johns Hopkins Medicine that would identify patients with prediabetes, help them better manage their condition and offer referrals to DPPs.


