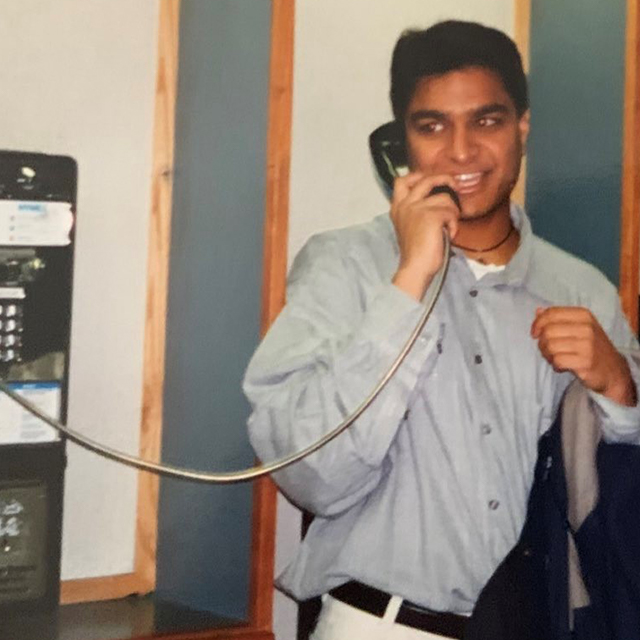
In 2019, Ashish Thakrar (Barker, 2017) was making rounds on a Johns Hopkins Hospital medical unit when he noticed a pattern: Internal medicine teams were not consistently treating and discharging patients with medications for opioid use disorder that reduce drug use and prevent potentially fatal overdoses. “In that moment,” Thakrar recalls, “I knew I needed to address barriers among doctors to help these patients start buprenorphine maintenance,” a prescription drug that treats addiction to heroin and other opioids.
Thakrar’s efforts became the focus of his quality improvement (QI) project for Pathways, part of the Osler Medical Residency Program. His work has created the successful Buprenorphine Bridge Team, which continues to support patients at high risk for overdose.
The project is one of dozens that Osler residents have championed since Pathways debuted in 2015.
As Osler Medical residents consider their future careers, the Pathways program continues to provide structured opportunities and mentorship to help residents get a jumpstart on their specialized areas of interest. These include physician-scientist, patient safety/quality improvement, global health and medical education.
Of the 150 residents in the Osler Medical Residency, about 50 choose to participate in Pathways, says Sanjay Desai, who directs the Osler Medical Residency. All pathways have formal curricula that include partnerships and boot camps with other university programs, including the Armstrong Institute for Patient Safety and Quality, the Bloomberg School of Public Health, and the undergraduate university. Residents interested in patient safety, for example, learn Lean Six Sigma, a strategy to improve performance and reduce variation, taught by Armstrong Institute faculty.
A Multifaceted Approach
Cultivating and reinforcing knowledge in each pathway requires a combination of learning approaches, explains Desai. “Pathways has been highly successful,” he says, “because we have identified faculty to mentor trainees and have also carved out space and time to help them meaningfully gain exposure and develop skills.”
Here’s how Pathways works: Initially, interns apply for specific pathways at the end of the year and are selected by senior faculty for their strong aptitude in a particular area. Trainees then incorporate one-on-one coursework, participate in group “boot camps” and begin hands-on experiences, such as practicing effective clinical research methods or improving teaching skills (for the medical education pathway). The program culminates with a research project that involves doctors, nurses, pharmacists and other departments across the health system.
That work can have enduring impact, notes Sara Keller (Thayer, 2010), who leads the patient safety/QI pathway. “Ashish’s QI project has proven transformative,” she says. “It made it possible for housestaff to prescribe the meds and be available to write prescriptions for people with opioid use disorder who are ready to be discharged.”
Keller also credits “the many great resources” at Johns Hopkins to support trainees, as well as infrastructure in the Department of Medicine. It’s been especially gratifying, she says, “to work with residents in the era of COVID-19, which created unprecedented challenges.” These include new institutional protocols, such as donning and doffing personal protective equipment, as well as communicating with families almost exclusively virtually.
Likewise, instruction in the global health pathway has been difficult. Normally, residents who choose this pathway spend six to eight weeks in Uganda, India, Peru or South Africa, says Yukari “Yuka” Manabe, who leads the pathway. Her work as associate director of Global Health Research and Innovation within the Johns Hopkins Center for Global Health has been limited to virtual instruction and research collaboration for trainees because of the pandemic.
Having lived in Africa for several years, studying infectious diseases, Manabe says she feels compelled to raise awareness about challenges she and her husband, who is also an infectious disease specialist, encountered, such as limited resources and cultural barriers. During safer times, she says, when trainees are able to travel abroad, “I want trainees to understand cultural frameworks, how to engage with patients, families and colleagues, and how to prepare for difficult scenarios. If residents can successfully engage in projects in resource-limited settings, they can learn effective leadership skills.”
Desai says he feels gratified to witness growing enthusiasm for the program — even among medical students. “They ask so many questions about the pathways,” he says. “It ends up being one of the most important things residency applicants are looking at.”
Expanded Reach and Interest
When Pathways debuted in 2015 at The Johns Hopkins Hospital, there were four to eight residents in each specialty area. Now, each pathway numbers 16 to 20 Osler trainees, says Desai. “The program continues to create and nurture leaders across the health care spectrum.”
In 2019, Desai incorporated the Johns Hopkins Bayview internal medicine residency into the Pathways program, and appointed Danelle Cayea, associate vice chair for education, to lead the program across the Department of Medicine. The medical education pathway, introduced in 2020, is the first bi-campus pathway, “benefitting from strong involvement from faculty and residents at both locations,” says Cayea.
Cayea adds she’s been pleasantly surprised by the program’s momentum. “We had to turn people away because we can’t accommodate everyone. Boot camps and intensive mentorship must take place during elective time. We need to figure out how to increase our capacity to meet the demands — that’s a good problem.”
She also notes that the Pathways program builds strong connections among faculty and residents.
Desai says the experience has already sparked an interest in duplicating Pathways across other training programs at Johns Hopkins, as well as at other institutions.
Desai is eager to next launch a data science and digital medicine pathway. These would focus on using big data to inform clinical questions and practice and study digital health transformation, including apps and wearable devices to improve health (see more on this specialty in the Q&A with alumni in this issue). “We continue to leverage everything Johns Hopkins has to offer to each of our residents,” he says.