Hypertension in the large vein that brings blood from the intestines to the liver is the main driver of cirrhosis. But when hepatologists need to know if the pressure in a patient’s hepatic portal vein is too high, they’ve mainly had to rely on indirect measurement methods.
Physicians eschew direct measurement of portal pressure due to its invasiveness. Instead, they determine the pressure of two nearby veins and use the gradient to estimate portal pressure. Typically done by threading a guide wire through a vein in the neck, this method is also fairly invasive.
Olaya Brewer Gutierrez says it’s time for some direct answers.
The Johns Hopkins gastroenterologist and endoscopist recently performed Maryland’s first endoscopic ultrasound (EUS) measurement of a patient’s portosystemic pressure gradient. Brewer Gutierrez hopes it’s the first of many.
“When liver doctors need to know whether a patient is at risk for cirrhosis or cancer,” she says, “we can now use EUS to see for ourselves.”
The Johns Hopkins therapeutic endoscopy team uses a new, tiny manometer connected to a small needle that provides a real-time, direct reading of the hepatic portal vein pressure — the most effective way to determine a patient’s risk for a host of dangerous liver diseases.
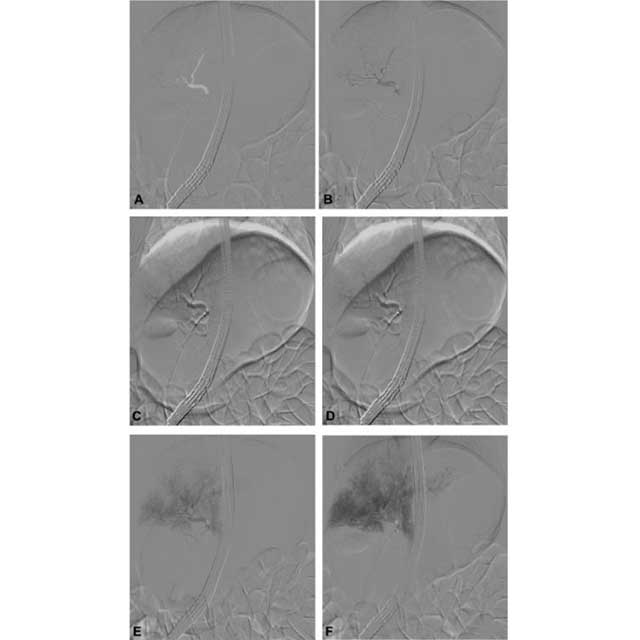
Brewer Gutierrez says EUS allows her to access the liver by way of the stomach. Through an endoscope, she inserts a 25-gauge needle into the patient’s middle hepatic vein. The needle is attached to a thin tube, the other end of which is attached to the compact manometer. She pushes a few drops of a heparinized saline flush into the vein and waits for the meter to settle on a pressure reading. Without removing the needle, she calculates the average of three readings for a final pressure number. The process is then repeated in the umbilical portion of the portal vein and, finally, a gradient is obtained.
Brewer Gutierrez wants liver doctors in the Mid-Atlantic region to know that, in addition to the direct readings of portosystemic pressure, she and her therapeutic endoscopy colleagues offer other diagnostic services without the patient having to visit more than once.
“We can do many different things in the same session,” she says. “We don’t have to bring the patient back or sedate them again and again.”
Brewer Gutierrez gives examples of what they can tell hepatologists about their patients.
“We can do an upper endoscopy, to see if the patient has esophageal varices,” she says, referring to enlarged blood vessels in the organ that leads from the mouth to the stomach. The condition is a symptom of liver disease and can result in dangerous bleeding.
During the endoscopic session, says Brewer Gutierrez, she can switch to endoscopic ultrasound “and assess the liver, right in front of you. Now we can see the shape of the organ, the characteristics of the parenchyma. We can see if there are nodules, which would suggest cirrhosis. We can see the edges of the liver and look for changes that indicate cirrhosis or lesions. We can compress the organ with the scope to determine the stiffness. We can even perform a liver biopsy.”
Brewer Gutierrez says Maryland’s first EUS measurement of hepatic portal vein pressure spared a patient from having a double transplant.
“The patient was in end-stage kidney disease,” she says, “and also had been diagnosed somewhere else with cirrhosis.”
In the work-up before a kidney and liver transplant, Brewer Gutierrez used EUS to find that the patient’s portal pressure was normal.
“It was less than 5 millimeters of mercury,” she says, explaining that a manometer reading between 5 and 10 millimeters indicates subclinical portal hypertension.
While the patient was sedated in the endoscopy suite, Brewer Gutierrez looked for other signs of liver disease.
“We didn’t find any lesions or nodules,” she says. “No esophageal varices. Nothing. We were happy to tell the transplant team that the patient only needed a kidney transplant. The liver was fine.”