The Johns Hopkins Heart and Vascular Institute provides the full gamut of advanced therapies for patients with mitral valve disease, says James Gammie, cardiac surgeon and the institute’s co-director.
“We have a team approach where cardiologists, cardiac surgeons, cardiac imaging specialists and others work closely to tailor medical therapy or recommend transcatheter intervention or surgery,” Gammie says. “We are innovators and leaders in this field, and our high-volume program yields beneficial outcomes.”
Several surgical procedures are available, says Gammie. Unique to Johns Hopkins, mitral valve translocation is for patients who have functional or secondary mitral regurgitation, and whose mitral valves become distorted by an enlarged ventricle.
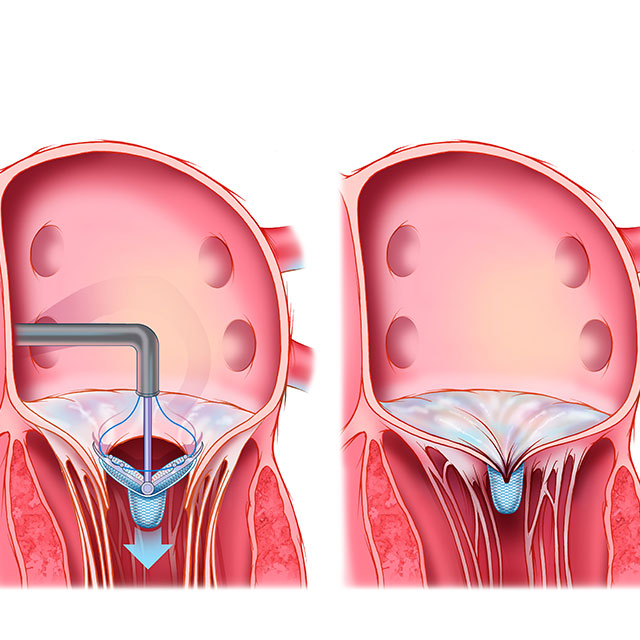
Normally, when the heart squeezes, the two mitral leaflets come together and snap shut like a double door, Gammie says. But with functional mitral regurgitation, an enlarged ventricle tethers the two leaflets of the mitral valve down into the ventricles. When the heart squeezes, the leaflets don’t come together, resulting in a large leak in the middle. Another version of the problem can be caused by an enlarged atrium.
During the translocation procedure, the intact mitral valve is detached. Then, surgeons sew in a 1-centimeter ring-shape patch, made of cardiac sac tissue, between the mitral valve and its typical base. This releases the tethering and enhances the leaflets’ ability to come together normally. The procedure has been done for 23 patients to date, with results for the first 15 patients published recently in The Annals of Thoracic Surgery. So far, the procedure has improved the leaflets’ ability to meet, with no postoperative mortality, stroke or renal failure.
Gammie and his research team are optimistic that this repair will be more durable than conventional repair techniques. “Our assessment shows that translocation results in more overlap between the two leaflets,” Gammie says, “and this in turn is likely to protect against failure in the mid and long term.”
Another approach to repairing the mitral valve is through repair of the chords. Imagining the mitral valve as a parachute with one or two broken cords, Gammie says, surgeons leave the canopy in place and replace the broken or stretched cords with expanded polytetrafluoroethylene (ePTFE), a thin synthetic material. Chordal repair with ePTFE now has a greater than 30-year history of durability, Gammie says.
For the 20% to 30% of patients with mitral valve disease who have atrial fibrillation, surgeons offer an add-on procedure during which surgeons use cryotherapy to make several scar lines in the right and left atria to halt irregular electrical impulses. Leaky tricuspid valves also can be repaired during mitral valve procedures by placing a collar around them.
Besides surgery, minimally invasive transcatheter options are available for mitral valve replacement and repair, particularly for patients who are elderly and not good surgical candidates, says interventional cardiologist Jon Resar, medical director of Johns Hopkins’ structural heart disease program.
One option for mitral valve repair uses a MitraClip, a device that is approved by the Food and Drug Administration. During the procedure, cardiac specialists use a catheter, threaded up to the heart through a vein in the groin, to deliver a dime-size device that clips the two leaflets of the mitral valve together and significantly reduces leaking of the valve. Echocardiographic guidance allows experts to verify results of the procedure as they perform it. Patients stay in the hospital for one night and have a follow-up echocardiogram the next day to ensure the clip is working well.
Resar and colleagues also are participating in a clinical trial of transcatheter mitral valve replacement for patients with severe symptomatic mitral regurgitation. This, too, uses a catheter, threaded up to the heart through a vein in the groin, to replace the leaky mitral valve with a prosthetic valve.