With the leading cause of maternal morbidity being cardiovascular disease, the Johns Hopkins Cardio-Obstetric Clinic launched in 2020 to care for patients who are pregnant or anticipating pregnancy and who have heart conditions or major cardiovascular risk factors. Research shows women who experience the onset of cardiovascular disease during pregnancy or who have adverse pregnancy outcomes have an increased risk of postpartum cardiovascular events.
The cardio-obstetric team performs a comprehensive review of each patient’s cardiovascular risk, monitors existing heart conditions, and identifies and treats any cardiovascular changes that occur during pregnancy or postpartum. Johns Hopkins physicians from maternal-fetal medicine, fetal therapy and cardiology work side by side to optimize maternal cardiovascular health and improve maternal and fetal outcomes.
The clinic has 40–50 patients at a time, with 20–30 who have conditions such as severe valvular disease, cardiomyopathy and complex congenital heart disease, and 15–20 with intractable hypertension and/or familial lipid disorders. These women are at the highest risk of adverse pregnancy and cardiovascular outcomes, including preeclampsia. Jason Vaught, a maternal-fetal medicine expert and director of labor and delivery at The Johns Hopkins Hospital, aims to coordinate care between the fetal therapy center and the cardiology department for these high-risk women.
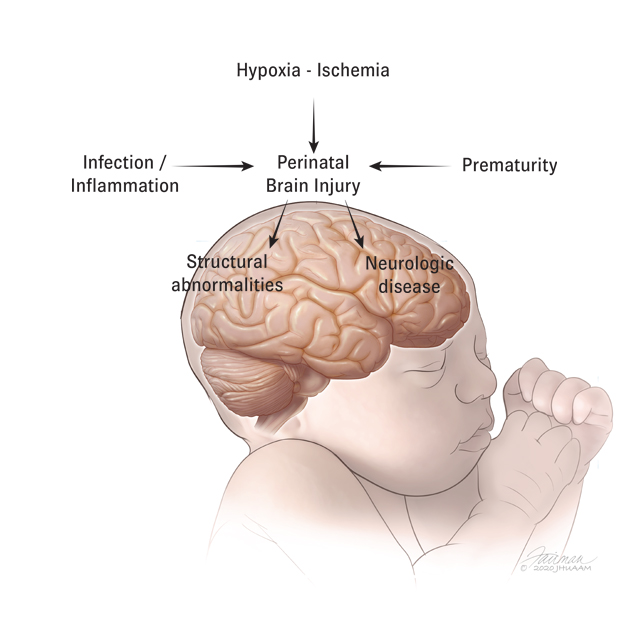
Ahmet Baschat, director of the Johns Hopkins Center for Fetal Therapy, says, “It’s not just about managing established disease better, but trying to prevent disease.”
A unique aspect of the clinic, says Baschat, is a personalized risk assessment for preeclampsia, early preeclampsia or intrauterine growth restriction. If a woman is at high risk for preeclampsia, Baschat employs aspirin at the right time and dose to prevent preeclampsia in 60% to 80% of cases.
When appropriate, the cardio-obstetric team coordinates with Johns Hopkins reproductive endocrinology and infertility experts before conception to establish care and to assess patients for in-vitro fertilization. Pre-pregnancy is also the time when a cardiologist who specializes in cardiovascular health in women, such as Anum Minhas, may replace certain cardiac medications with alternatives that have a better safety profile during pregnancy and lactation.
When needed, the doctors have the capability to perform cardiac monitoring and invasive arterial line monitoring in Johns Hopkins’ labor and delivery unit, so that women with severe valvular disease or other complex congenital heart disease will not have to go to the critical care unit for delivery. The nearby neonatal intensive care unit can handle newborns who are less than 24 weeks gestation.
“It feels really good to be part of a group of like-minded individuals in fetal therapy, cardiology and maternal-fetal medicine,” says Vaught. “The cardio-obstetrics program is a year out, and some patients have already talked about getting pregnant again.”