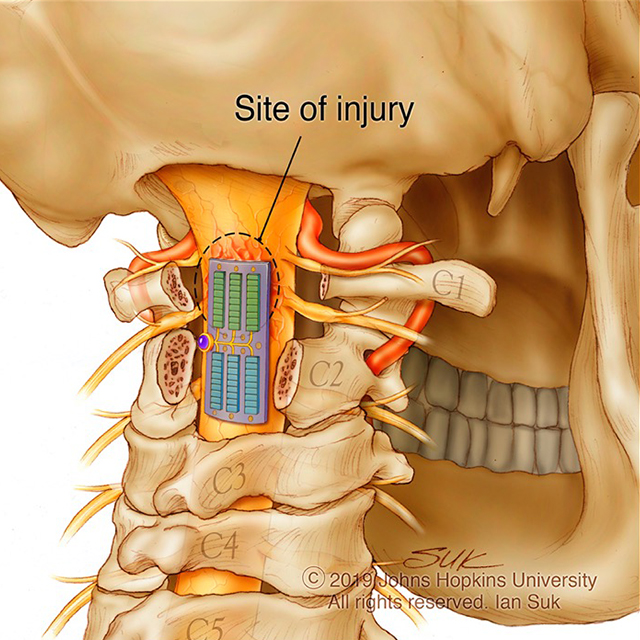
Johns Hopkins neurosurgeons have performed the institution’s first augmented reality surgeries for living patients. During the first procedure, on June 8, 2020, the physicians placed six screws in a patient’s spine to fuse three vertebrae in order to relieve debilitating back pain. For the second surgery, on June 10, surgeons removed a cancerous tumor from a spine. The doctors report that both patients are doing well.
The technology that the physicians used for the augmented reality surgeries consisted of a headset with a see-through eye display that projects images of the patient’s internal anatomy, such as bones and other tissue, based on CT scans — essentially giving the surgeons X-ray vision.
“When using augmented reality in the operating room, it’s like having a GPS navigator in front of your eyes in a natural way, so you don’t have to look at a separate screen to see your patient’s CT scan,” says Timothy Witham, director of the Johns Hopkins Neurosurgery Spinal Fusion Laboratory and professor of neurosurgery at the Johns Hopkins University School of Medicine. Witham led the 2020 spinal fusion surgery.
Augmented reality has been used for several years to train medical students for surgeries such as blood clot removal and penis implant.
The University of Alabama, with Emory University, piloted orthopaedic shoulder replacement using Google Glass, and Stanford University is developing its own device. The device used in the surgeries at Johns Hopkins is manufactured by Augmedics, a company based in Israel. Witham and colleagues at Johns Hopkins began working with the company last year to pilot a new augmented reality headset. They tested the device by implanting screws in the spine of a cadaver.
Read the entire version of this article: “Johns Hopkins Performs Its First Augmented Reality Surgeries in Patients.”
COI: Witham is a private consultant for Augmedics, and is compensated for consulting services regarding stock options. The Johns Hopkins University School of Medicine manages these arrangements in accordance with institutional conflict of interest policies.