New Individualized Care Options for All Stages of Prostate Cancer
The Johns Hopkins Kimmel Cancer Center at Sibley Memorial Hospital offers comprehensive, multidisciplinary care and the latest treatments.
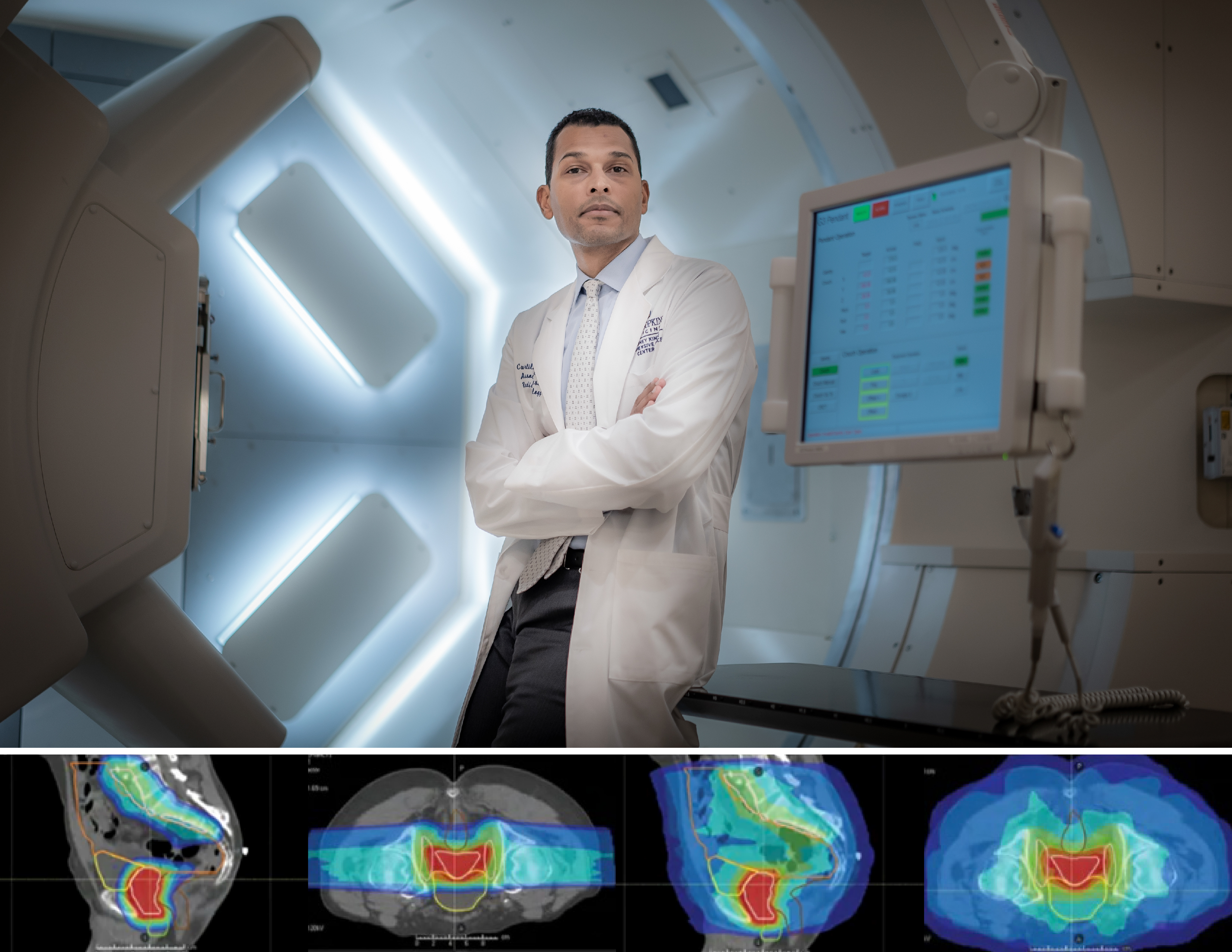
Top: Curtiland Deville, M.D., medical director of the Johns Hopkins Proton Therapy Center at Sibley Memorial Hospital. Above: The example shows how a patient’s bowel, bladder and rectum are spared of radiation in proton therapy (left photos) versus photon radiation therapy (right photos).
New, advanced treatments for prostate cancer provide patients with a multitude of options. Curtiland Deville, M.D., medical director of the Johns Hopkins Proton Therapy Center at Sibley Memorial Hospital and co-director of the Johns Hopkins Kimmel Cancer Center Prostate Multidisciplinary Clinic at Sibley Memorial Hospital, says that the team works with each patient to identify the most appropriate individualized care for their specific case.
Prostate Cancer Multidisciplinary Clinic
The multidisciplinary clinic gives patients access to the most advanced treatments and to clinicians in a variety of specialties, who work together to determine the best course of treatment.
In these bimonthly clinics, a patient meets in the morning with a urology or radiation oncology resident or nurse practitioner. The patient’s case is then reviewed by a team that includes a urologic oncologist, a medical oncologist, a radiation oncologist, a radiologist and a pathologist. The relevant physicians then each meet with the patient in one-on-one sessions the same afternoon to discuss the diagnosis and management options.
“It’s a patient-centered approach where they can get a consultation with everybody who would be involved with their prostate cancer diagnosis and management,” Deville says. “The patient can be evaluated and have a treatment plan in place all in one day.”
The multidisciplinary clinic also includes research coordinators, research trial specialists and social workers who can help patients navigate the clinic and their diagnosis. Patients also have access to novel treatments through clinical trials that are often not available elsewhere.
“Ultimately, what we strive to bring as Johns Hopkins faculty is the clinical and research expertise to look at the whole picture and make sure you’re getting the best care with all of the most advanced and best available tools to treat prostate cancer.”
Curtiland Deville
High Dose Rate Prostate Brachytherapy
One possible treatment is high dose rate (HDR) prostate brachytherapy, a therapy that is offered at only a few specialized centers across the country and in the Baltimore/Washington region.
HDR brachytherapy offers patients an alternative to low dose rate (LDR) prostate brachytherapy, with less potential for radiation to be absorbed by surrounding tissues compared with other types of radiation. It involves depositing high-dose radiation directly into the prostate through a catheter for 15–20 minutes, while LDR brachytherapy involves placing permanent radioactive seeds in the prostate that slowly release radiation over time. Thus, with HDR, the patient does not leave the clinic with implanted radiation or have radiation safety precautions and limitations from being radioactive.
“In radiation, we’re always looking to minimize exposure of normal tissues,” says radiation oncologist Rachit Kumar, M.D., who is building the HDR prostate brachytherapy program. “Doing this allows us to be very focused with that radiation, and to do so in such a way that minimizes exposure to normal tissues while still providing a really high dose of radiation to the target.”
HDR brachytherapy can be used to treat early-stage prostate cancer as a solo treatment, or for patients with high-risk or locally advanced disease, it can be given in combination with external beam radiation techniques such as intensity-modulated radiation therapy or proton therapy. It is especially useful as a “salvage” therapy for patients whose cancer has recurred in the prostate after a prior course of radiation.
Studies show that results are similar to those in LDR brachytherapy, with 90%–95% of early-stage patients having no recurrence for at least five years after treatment. Ninety percent of patients go home without needing a catheter in their bladder, and of those who do, it is usually removed within two days.
Advanced Imaging and Image Guidance
The Johns Hopkins Kimmel Cancer Center at Sibley offers the latest imaging and image-guided treatments. This includes multiparametric MRI, an advanced imaging technology that can detect prostate cancer; MR simulations, which help clinicians plan radiation treatment based on the location of tumors; and a targeted biopsy system that allows for specific targeting of tumors. It also offers molecular imaging such as the prostate-specific membrane antigen (PSMA) PET-CT, which is more sensitive in detecting cancer that has spread to distant organs or lymph nodes than conventional imaging with a CT scan or bone scan.
For eligible patients undergoing radiation, the clinic offers hydrogel spacers, which are injected between the prostate and rectum prior to patients receiving radiation in order to reduce side effect risks to the rectum.
Proton Therapy
Sibley is also home to the Johns Hopkins Proton Therapy Center, which treats a high volume of prostate cancers, says Deville.
Proton therapy can benefit patients with localized or postoperative prostate cancer as well as those with advanced disease. The treatment involves high-energy, precisely targeted particle beams that deposit radiation directly in the targeted tumor, which limits collateral exposure to surrounding tissues and organs, such as the bowel, rectum and bladder. The center also uses advanced imaging to ensure the protons are hitting their target, including a new technology known as RGPT (real-time image gated proton therapy) that shuts off the beam if it moves out of a 2-millimeter threshold from its target.
Radiopharmaceutical Therapy
The center has a radiopharmaceutical program that offers Radium-223, also known as liquid radiation. Administered through an IV infusion, Radium-223 is given to patients with metastatic prostate cancer that has spread to the bones and has shown resistance to hormonal therapy. Recently, the center began offering lutetium therapy, which is also delivered through an IV, and treats prostate cancer that has spread to other parts of the body beyond the bone.
With the variety of prostate cancer treatment options available, Deville says his team’s goal is to present the best treatment options for each patient.
“These are not competing tools,” he says. “Ultimately, what we strive to bring as Johns Hopkins faculty is the clinical and research expertise to look at the whole picture and make sure you’re getting the best care with all of the most advanced and best available tools to treat prostate cancer.”
Learn more about Johns Hopkins cancer specialists in the National Capital Region at hopkinscancerdc.org.
