Patient Access Line Marks 10-Year Anniversary
Team of experienced nurses strives to make sure patients understand discharge instructions.

Since 2013, a group of nurses with extensive and varied clinical experience has staffed a telephone call center, making sure that patients recently discharged from one of three Johns Hopkins hospitals understand and are able to follow the instructions from their care teams.
This past July, the Patient Access Line (PAL) celebrated 10 years of helping patients follow their care instructions and avoid the need for readmission to the hospital. In the decade since it was established, PAL has expanded its services from 21 units at The Johns Hopkins Hospital (JHH) to 49 units across JHH, Johns Hopkins Bayview Medical Center and Johns Hopkins Howard County Medical Center.
Diane Lepley is the senior director of care coordination health policy and outcomes at The Johns Hopkins Hospital and director of the PAL program. According to Lepley, services that provide highly specialized care such as organ transplants, cardiac surgery and others may call their patients after they’re discharged as part of the transition from hospital to home.
“But they’re not the only home-bound patients who can benefit from a standardized post-discharge phone call to review and reinforce discharge plans,” says Lepley. “To promote seamless care transitions, the PAL team connects with patients who might not otherwise receive a call.”
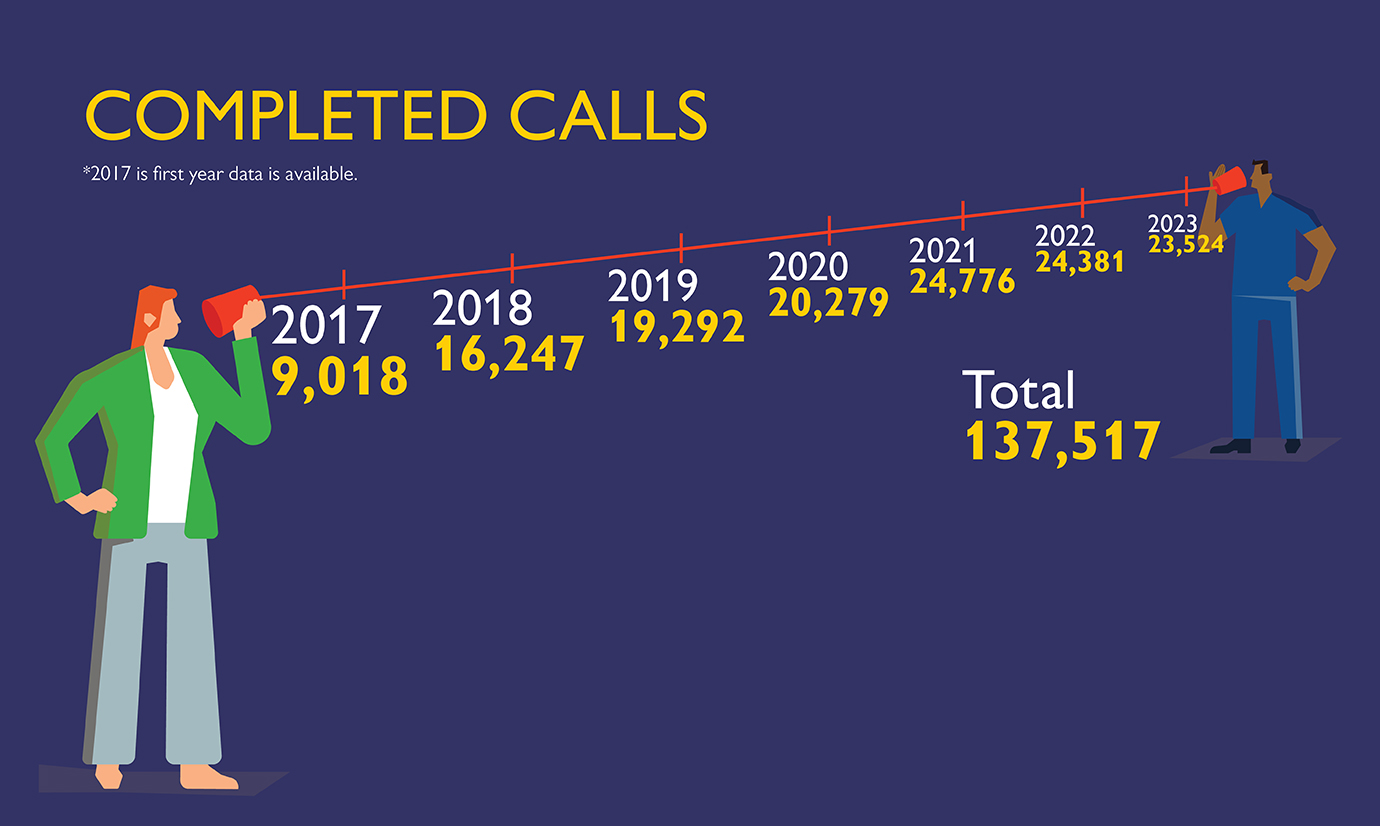
In fiscal year 2022, the 10-nurse PAL team spoke with more than 24,000 patients — or almost 80% of eligible patients — to help them understand their after-care instructions. Since PAL began its current data collection in 2017, its full-time nurses have completed nearly 140,000 phone calls. According to PAL data, patients who get a phone call from a PAL nurse are 30% less likely to be readmitted to the hospital.
“We have to know at least a little bit about all sorts of things,” says Missie McAdam-Cox, a PAL team leader who has been a nurse for 32 years, the last 21 of which have been at Johns Hopkins. Like most of the PAL nurses, her work on different units at JHH and Johns Hopkins Bayview has provided varied and broad experience.
McAdam-Cox says PAL nurses come from different nursing backgrounds “so we can tap into each other’s experiences.”
“I loved working and learning in different areas,” she says. “Recovery, IV therapy, GI-endoscopy, lots of ICUs … I’ve always been excited to try new things.”
As an example, McAdam-Cox cites a recent case in which a Spanish-speaking man in his 40s was admitted to Johns Hopkins Bayview with symptoms of untreated type 2 diabetes. During his stay, his care team explained his condition and showed him how to treat it. A physician prescribed medicines, and the man was discharged two days after he was admitted.
The day after his discharge, however, the symptoms that sent him to the hospital returned. Fortunately, the man received a phone call from McAdams-Cox at PAL, who spoke with him through a medical interpreter.
“It wasn’t until he got home that he realized he couldn’t afford any of the medications he was prescribed,” she recalls. “He said he was embarrassed to tell his care team at the hospital” about his financial situation.
PAL nurses are well-versed in the many resources available to Johns Hopkins patients. After speaking with the man, McAdams-Cox secured his medications through a program for patients with low incomes. During their conversation, she also learned that the man does not have reliable transportation. By the end of the phone call, McAdams-Cox had not only secured low-cost medications to help him manage his diabetes, she also arranged to have them delivered to his home.
"He was so grateful," says McAdams-Cox. "That kind of call happens really often. We're usually able to link people to resources when they need them."
Sharon Schromsky, a PAL nurse with 28 years experience at Johns Hopkins, says that an overnight hospital stay can be disorienting and exhausting. When it comes time for post-discharge instructions, patients can miss important information.
"I mean, they're in the hospital so they're not quite at their best, even when they're getting discharged," she says. "There's only so much information a person can take in, even on their best day."
PAL's origins stem from a Centers for Medicaid and Medicare Services Innovation (CMMI) grant awarded to Johns Hopkins Medicine in 2012. The $20 million led to the formation of the Johns Hopkins Community Health Partnership, or J-CHIP, which was a regional care coordination model aimed at reducing hospital readmissions and improving health outcomes with hospital and community-based interventions.
"By 2013, just months after the grant announcement, PAL was up and running as one of our bundle of strategies," says Lepley.
Some readmissions are unavoidable, but many are not. McAdams-Cox says that one in three 30-day readmissions occur within seven days of discharge, which can be an indicator that the patient is not following post-discharge instructions.
"That's still the primary goal — to prevent readmissions," she says. "But [PAL has] evolved a lot in 10 years."
In addition to the benefits to individual patients and to the hospital bottom line, PAL has helped solve other problems. Each call generates data in the Epic electronic medical record system, allowing PAL nurses and hospital administrators to spot trends among discharged patients.
For instance, PAL provided the data that led to a recent quality-improvement initiative to reevaluate the way medications are documented in Epic. Data collected from PAL phone calls helped identify opportunities to better communicate medication information with patients.
"Let's say a physician tells a patient to take Tylenol for pain," says Schromsky. "But other times, they might call it acetaminophen, since that's the pain-relieving ingredient in Tylenol. Sometimes that can get confusing for patients."
PAL's Shavona Jones is in her 17th year as a nurse at Johns Hopkins. She recalls a recent conversation with an out-of-state patient who traveled to Johns Hopkins for a surgical procedure. Two days after the patient arrived back home, she experienced intense post-surgical pain, despite following her medication instructions.
"The woman told me she was improving, but that she was in a whole lot of pain," Jones remembers. "She couldn't sleep, couldn't get comfortable. It sounded weird to me, since she was on a pain medication that's usually pretty effective."
"But it turned out she'd been taking a dose that was far too low. She was taking the pre-surgical dose and somehow she missed that there was a stronger prescription for after her surgery. I was so glad we could help her."
