Not every nurse gives medications by IV infusion every day, and while the mechanics seem straightforward, any oncology nurse will tell you that doing it safely and successfully takes special expertise and skill.
“Giving an infusion, it’s about being there, being present. You give them the medication and you stay front and center. You’re watching how they breathe, having a conversation with them, all while checking their color, blood pressure, looking for skin prickles — anything that might indicate any issues,” says Jamie O’Connor, B.S.N., R.N., O.C.N., a clinical nurse who is part of the Johns Hopkins Kimmel Cancer Center outpatient infusion team at Sibley Memorial Hospital.
When it became clear that monoclonal antibodies given by IV infusion could protect people with COVID-19 at high risk of getting severely ill, these oncology nurses were crucial leaders in the discussion and planning about how best to administer the treatments.
A multidisciplinary team formed to serve these patients as safely and effectively as possible. In addition to oncology nurses, the group also included intensive care nurses, emergency department nurses and providers, pharmacy, admissions, information technology and hospital leadership. Utilizing the Department of Defense’s Operation Warp Speed playbook as a guide, the team leveraged strengths across the health system i to get the systems and processes in place as quickly as possible.
The team quickly finalized a plan to create a clinic within the emergency department, which already met the federal and District of Columbia regulatory criteria for serving patients with COVID-19. To get people treated as soon as possible, infusion center nurses, the experts in giving these monoclonal antibody treatments to vulnerable patients, would deliver the care.
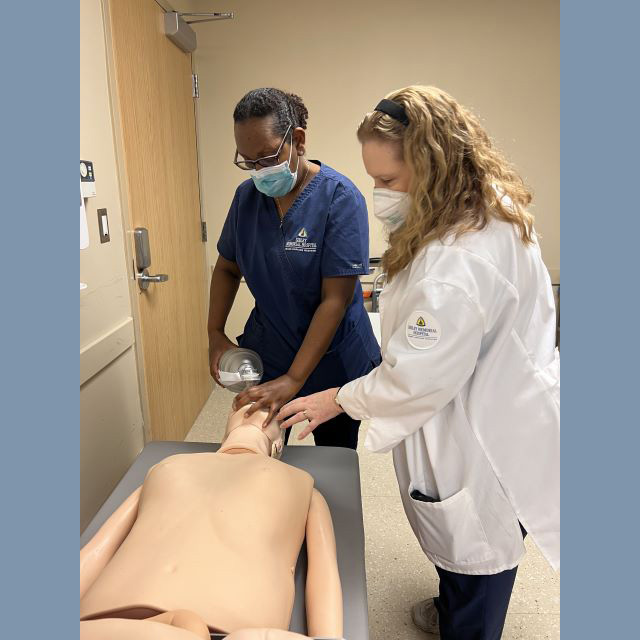
“Bringing together this team and tapping the expertise of oncology nurses was novel at the time, but also important for the safety of the patients,” says Onyinye Mkparu, M.S.N., M.B.A., R.N., O.C.N., nursing director for oncology. “Monoclonal antibodies to treat COVID-19 were only under an emergency authorization for use without full FDA approval. There was a lot we didn’t know about this treatment and a lot we were still learning about COVID-19 and how it affects very vulnerable patients. We needed our very best infusion nurses to do this work.”
O’Connor, a seasoned oncology nurse with exactly the experience the team needed, was one of the first people to step up and volunteer.
“Through the pandemic, oncology nurses were doing everything they could to avoid exposure to COVID-19 so they could protect their vulnerable cancer patients from exposure,” says Katie Evans, B.S.N., R.N., O.C.N., nurse manager in the infusion center, who also helped launch the clinic and administer care. “But when the need arose for someone with our expertise to jump in and help these patients in need, Jamie was ready right away to do what needed to be done."
She has built relationships and collaborations with people in every department to keep the program running smoothly. She continues to administer monoclonal antibody infusions to patients with COVID-19 and also trains others on how to do it safely. Some days, she finishes with her patients with COVID-19 , undergoes a thorough decontamination process, and then goes back to the Kimmel Cancer Center to give infusions to those patients, too.
The oncology nurses’ willingness to help because patients needed them led Sibley to be the first hospital in the Johns Hopkins Health System to deliver monoclonal antibodies to patients in this way. To date, over 120 patients have been treated with monoclonal antibodies at Sibley.
O’Connor, with her manager Evans’ support, has been the real champion for this process and for the care delivery that happens, according to her colleagues.
Nursing Director Mkparu attributes the program’s successful outcomes to “how much heart Jamie and the entire team have put into this process.”
And it’s true. Just like she does for her patients with cancer, Jamie follows the progress of her patients with COVID-19 even after they’ve left the clinic.
“The heart of an oncology nurse is that you are with people through thick and thin. I call them and see how they are doing, ask them about the things we talked about during their treatment — did they go on that trip they talked about? I’m a nurse, I never meet anyone on their best day. I love hearing about the things they are able to do today that they couldn’t do before.”