Illustration by Michael Woloschinow
One night last fall, Pierre Gibbons ran into a burning building to help a neighbor — and emerged with severe burns and very slim odds for survival. In their efforts to give Gibbons a fighting chance, specialists at the Johns Hopkins Burn Center tried a one-two punch they’d never used before.
The Gibbons family enjoyed an idyllic day together before their trial by fire began. Like most families, they don’t gather as often as they’d like. When they do, things don’t always go smoothly. But that Sunday afternoon in September was different, which is one reason siblings Jeremiah and Taylor Gibbons remember it so vividly.
“It was kind of surreal,” says Jeremiah, the birthday-boy center of attention that day. “For whatever weird reason, every little interaction seemed totally heartfelt.”
A second reason that memory looms so large is that the family’s life turned upside down the following day. When Taylor’s phone rang at 10:30 p.m. that Monday, Sept. 22, 2019, she did a double-take: Why in the world would one of her father’s friends be calling?
“Taylor, your Dad’s been burned. He’s at Johns Hopkins Bayview. You should go there.”
She lives an hour away. She alerted Jeremiah, who is much closer. He and his wife, Rachel, had missed calls from that friend while taking advantage of a brief sleeping window that opened when their newborn son dozed off. Jeremiah raced over with no idea what was going on, but as a Baltimore City firefighter, he grasped the gravity of the situation when he saw how the brotherhood had gathered. A fleet of ambulances and fire trucks were outside the Emergency Department of Johns Hopkins Bayview Medical Center. He spotted two deputy chiefs, one from fire, another from emergency medical services.
“I got out, didn’t even think about where I was parking,” Jeremiah recalls. “Everyone was like, ‘Oh my God, oh my God.’ They were all crying.”
Jeremiah started crying too. When he found his father — burned body wrapped in blankets, eyes glazed but open — he put a gentle hand on his forehead and said the only words that came to mind. “Hey, Dad, I’m here for you, man.” Later, a paramedic would tell Jeremiah how his dad had shouted, “Jeremiah Gibbons! Engine Six!” over and over during the ambulance ride to Johns Hopkins Bayview.
The patient was wheeled away to the ICU in the Johns Hopkins Burn Center. Taylor arrived. The siblings were directed up to the Burn Center to await word on their dad’s condition. Talking with first responders that night, Taylor and Jeremiah started to piece together what had happened.
Pierre Gibbons, 57, had been watching Monday Night Football with his friend. Hearing a ruckus outside about flames in a nearby house, both went to investigate. While his friend checked out back, Gibbons headed out front where, through an open front door in the rowhouse on fire, he saw his 77-year-old neighbor, Mary Sterling, waving for help.
In a scene captured in a grainy cellphone video that soon went viral online, Gibbons marched inside the burning rowhouse. He almost made it back out with that elderly neighbor in his arms, collapsing just short of the front-door finish line. Both were alive when firefighters reached them, but barely. Sterling would die several weeks later.
Johns Hopkins Burn Center surgeon Julie Caffrey didn’t sugarcoat things when she talked with Jeremiah and Taylor that night. After some basic triage work — intubating the patient, cleaning wounds and surveying damage — she reported that burns covered 65 to 70 percent of their father’s body. In such cases, burn specialists run an algorithm that tallies historical survival numbers for patients with similar ages, burns and lung damage. The mortality rate for Gibbons approached 90 percent.
Listening, the siblings tried to get their heads around two big things: Their dad had played the role of hero, and he was probably going to die because of it.
“Go home and get some sleep,” Caffrey said. “You’ve got some long days ahead.”
Journey to Recovery
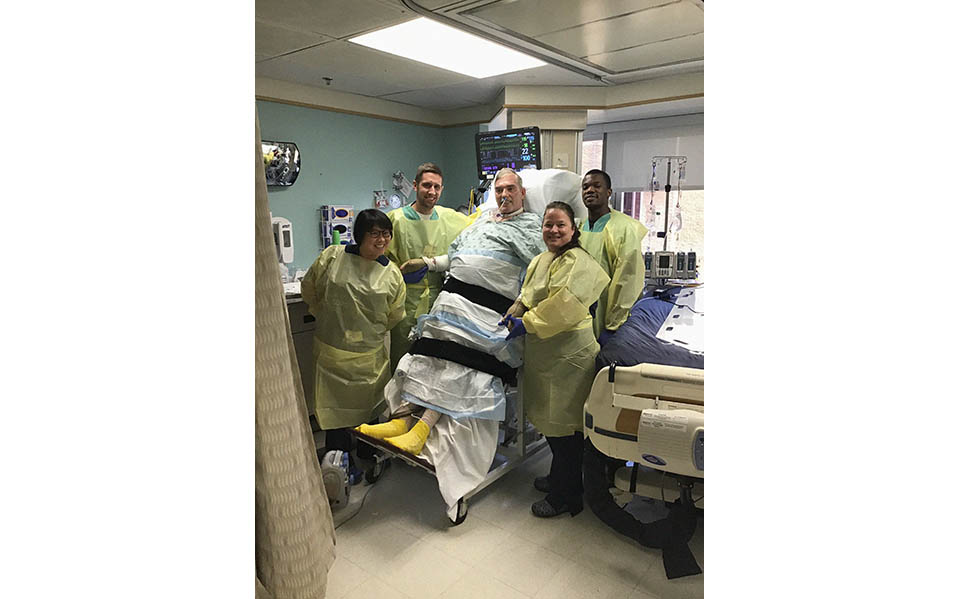
Photos from the Gibbons family album capture Pierre and family members before the fateful fire, and at key times throughout his monthslong recovery at the Johns Hopkins Burn Center.
Photos Courtesy Gibbons Family
Dismal Odds
Strange as it may sound, Gibbons got lucky that night. Located seven minutes from his home in the Patterson Park neighborhood of Baltimore City, Johns Hopkins Bayview houses an elite academic burn center where three surgeons and a small army of specialists across many disciplines — nursing, psychology, intensive care, chaplaincy, social work, nutrition and physical therapy among them — take on the most daunting cases the specialty has to offer. The center treats about 800 burn patients a year, half of whom are admitted to the hospital. Its physicians also provide outpatient treatments and surgeries for scarring and skin infections related to other wounds besides severe burns.
“The charge here, and really all across an institution like Johns Hopkins, is to define new standards of care, not just follow the existing ones,” says Scott Hultman, the center’s director. “What that means in practice is that we’re always pushing the boundaries, looking for new and better strategies.”
Gibbons put that mission to a stiff test. Burn Center surgeon Mohammed Asif ticks off a fast-and-furious run of complications that arose in the days that followed Gibbons’ arrival, including kidney failure, multiple strokes, skin graft rejection, drug-resistant pneumonia and pancreatitis. By the time of that last mishap, the dial on his mortality algorithm was up around 98 percent, Asif says.
“The thing is, algorithms like that are informative for populations of patients, but individuals are all different,” Hultman says. “We can’t really predict who’s going to live and who’s going to die at that individual level, which is why we can’t ever let those numbers get in the way of going all out for patients like Pierre.”
‘Our Father Is a Fighter’
The Gibbons family grabbed hold of this distinction like a lifeline. When Taylor and Jeremiah had met with Caffrey the morning after their dad arrived at the Burn Center, the surgeon had warned that the ordeal ahead would be arduous, perhaps six months in intensive care followed by two to five years of rehabilitation, much of it spent as a full-time inpatient. Pierre might regain a reasonably full measure of physical and mental functioning, but that best-case outcome was far from a sure thing.
The talk culminated in a stark question: Did Pierre’s children want doctors and nurses to go all out to save him?
The middle child of five, Pierre Gibbons had grown up outside of Washington, D.C. The family moved to Santa Fe, New Mexico, during Pierre’s high school years. His father, Dave Gibbons, describes that as a challenging period — the kids weren’t exactly on board with the move. But he was proud of the way Pierre moved forward in the face of that disappointment.
“It was quite something to see, how this Anglo kid from the East Coast who didn’t want to move found a way to fit in so quickly with all the Indian and Hispanic kids,” he says. “Pierre has always had a remarkable ability to meld with other people.”
Pierre spent four years in the Navy after high school. In the years that followed, he would marry, divorce and eventually move back to the Washington, D.C., area and establish himself as a facilities manager for commercial properties. Career opportunity brought him to Baltimore, where he most recently worked at MedStar Good Samaritan Hospital.
As a father, Pierre could be demanding. His children say they never doubted his love, but they also never doubted that he would expect them to meet the challenges and disappointments of life head-on.
“He is the toughest person I know, the scrappiest, hard-headed-est, old-school-est guy you’ll ever meet,” says Jeremiah, 34. “Everybody else is like, ‘I can’t believe he ran into a burning building.’ I’m like, ‘Oh, I can totally believe it.’”
Looking back, Jeremiah and Taylor, 25, feel like those childhood lessons in toughness had been delivered in preparation for the moment when they had to summon up their courage, look their father in the eye and ask him a life-or-death question. First things first, however: They told him they loved him. He mouthed their words back at them around his intubation tube.
Then Jeremiah put the question on the table: “Dad, do you really want to do this?”
Pierre’s eyes were clear. He understood. He nodded his head. Soundlessly, he uttered a single word, “Yeah.”
The Gibbons children told Burn Center physicians to go all out. Caffrey was struck during that exchange by the family’s confidence: “They were saying, ‘You don’t know this guy. Our father is a fighter.’”
On top of that run of strokes and organ failures, Pierre would undergo 24 surgeries over five and a half months in intensive care at the Burn Center. Every time the human body gets invaded by a scalpel, Caffrey notes, it goes into an inflammatory overdrive that sends waves of high-alert stress out in every biological direction.
“Here’s a guy in his late 50s, and basically what’s happening with his injuries and those surgeries is his organs are running a marathon nonstop for five or six months,” she says. “It takes a special person, with a special will to live, to survive that. There’s an element inside of Pierre that’s a big part of his success.”
One week into their family’s ordeal, Taylor and Jeremiah rushed to the Burn Center in response to an emergency summons. Their father had slipped into a coma. Technicians were scanning for brain activity to see if the fight was already over.
The wait to see if Pierre would emerge from the coma stretched past two weeks and into a third. By this point, the relatives who had driven or flown in from distant locales to offer support to Taylor and Jeremiah had returned to their lives.
“We came to a point,” Jeremiah says, “where we’re thinking, ‘Should we have done this? Would it be better to just let dad be in peace?’” He invited a fire department chaplain to come pray with the family.
One night, wracked by doubts, he sent Caffrey a late-night text: “Are we pushing it too far? Should we throw in the towel?” Caffrey replied, “What? No, of course not!”
As the third week of coma came to a close, the call came. “Get down here. Your dad’s awake.” Jeremiah got there first. His father’s eyes were open. He couldn’t talk, and he looked confused, but so what?
“Oh, my God,” he shouted. “Dad! You’re there!”
‘Like a Miracle’
The medical interventions that helped bring that day to pass are all over the map. Early on, kidney function is key for burn victims. Swelling caused by burn wounds leads to leakage of internal fluids at levels that can interfere with the supply of oxygen to vital organs. Unable to discharge enough liquids, Gibbons landed on continuous venous dialysis.
Another key is providing protective coverage to open wounds on bodies that have little or no skin. The standard-of-care treatment here is skin grafts using living tissue harvested from cadavers, which usually provide protection through a three-week-long healing window. Not so with Gibbons: Over and over again, his grafts failed within a couple of days, infected by the multidrug-resistant pneumonia and blood-related infections (bacteremia) in his body.
“To be honest,” Asif says, “we weren’t sure what to do at that point.”
Pushed beyond standard of care, Burn Center physicians tried a one-two punch they’d never thrown before. They used a pair of new products, a synthetic skin substitute called BTM (for biodegradable temporizing matrix) and ReCell, a device that grows new skin cells from a patient’s own tissue.
BTM is made with an inner layer of biodegradable polyurethane foam and an outer layer of impervious sealing material. It provides temporary wound coverage that won’t get infected with disease or come under attack by the immune system. As patients grow new skin during the BTM healing window, that skin grafts seamlessly to the inner layer. Once that happens, surgeons can peel off the outer layer like a bandage.
By coincidence, Burn Center physicians had sat through their first training session with ReCell just days before Gibbons arrived. Recently approved by the U.S. Food and Drug Administration, the device gives physicians a high-speed tool to expand the number of skin cells in a biopsied sample. This process used to involve sending samples to a lab and waiting three weeks, while ReCell accomplishes the feat on-site in an operating room in less than an hour. The cost savings are as impressive as the time savings.
“For a little less than $20,000,” Hultman says, “we were able to deliver treatments that would have cost $300,000 if we did it the old way.”
The soupy mixture that comes out of the ReCell machine doesn’t look anything like human skin, but it’s full of specialized skin cell types chosen for their robust immunologic qualities. The mixture is sprayed on or poured into wounds. In the case of Gibbons, those wounds were then covered with BTM.
“Almost overnight, his physiology changed,” Asif says. “We were hopeful about this strategy, but what happened was almost like a miracle, the way he started getting over his infections and regaining function in his kidneys.”
Burn Center physicians have high hopes that these two treatments will prove beneficial for future patients as well. They are now participating in a multisite randomized trial comparing BTM outcomes with standard-of-care treatments in a population of more than 200 patients. Here, too, the potential cost savings are significant: Caffrey says BTM is perhaps one-third less expensive than standard of care.
Later, Gibbons became the first Burn Center patient to use an advanced “tilt-table” hospital bed designed to prevent bedsores by giving caregivers a constant color-coded map showing a patient’s weight distribution across the mattress. That bed also rotates up a full 90 degrees, making it easier for bedridden patients to re-acclimate themselves to the vertical position and begin getting their legs ready to bear weight again. The device was donated to the Burn Center by a small nonprofit, Sons of the Flag; Hultman hopes that arrangement will lead to the purchase of additional tilt-table beds soon.
After emerging from his coma in October, Gibbons endured frequent episodes of delirium that seemed linked to intense dreams. Concerned about his sleeping patterns, Burn Center physicians sought advice from a team at The Johns Hopkins Hospital studying how ICUs can become more sleep-friendly operations. Those discussions led to a change to a quieter room location and alterations to Gibbons’ medication schedule.
“What makes this such an exciting place to work is that you’re in this environment of constant innovation, of trying new things, of pushing the edges,” Hultman says. “When that work comes together for a patient like Pierre, gosh, it’s a great feeling for everyone.”
In this case, those feelings extend far beyond the patient’s caregivers and family. Shortly after news broke about his heroic actions on the night of the fire, Gibbons became the focus of a remarkable grassroots campaign of public support. A Facebook page, Keep Fighting Pierre, surpassed 1,500 followers. A GoFundMe campaign to defray the medical expenses raised more than $50,000. Family and friends organized several fundraising events. At the Burn Center, cards and letters arrived for Gibbons from all over the country.
‘I Couldn’t Stand There and Watch Her Burn’
By the time I visited gibbons in mid-February, he’d made remarkable progress. Though still bedridden in the ICU, he was tackling an hourslong daily regimen of physical therapy. Even though he was still unable to use his left shoulder and arm, there were no signs of stroke aftereffects in his voice.
I told Pierre how his father, Dave, had shared a theory with me about the night of the fire. When he was in the Navy, Pierre did duty as a firefighter. Though nearly 40 years have passed, Dave suspects that military training kicked in for Pierre at some unconscious level.
“He’s probably correct about that,” Pierre says. “You know, I didn’t discuss with myself whether to go in or not. I just did it.” In a conversation with his son and daughter, he’d described this turn of events in blunter fashion: “I couldn’t stand there and watch her burn.”
He brushes aside the hero talk that has surrounded him since the night of the fire. Whenever it comes up, he tries to deflect attention onto the “real” heroes — firefighters and paramedics, physicians and nurses at the Burn Center. Thinking about the long rehab road ahead, he remembers a lesson he used to try and teach his kids: “There are consequences when you take actions.”
He laughs heartily: “I’m paying some consequences now, that’s for sure.”
Gibbons hopes that one mystery about his trial by fire becomes clear someday. Why did God let him live? What special plan or purpose does He have in mind for the rest of his days? In the meantime, he is trying to focus on lessons he’s already learned through this ordeal. Slow down. Stop being in such a rush to get to the next stoplight. Just be nice to people.
There have been days since their father came out of his coma when Jeremiah and Taylor found themselves wondering what happened to the grumpy part of their father’s personality.
“It’s almost like that grouchy guy is missing now,” Taylor says. “He’s been really cool and really kind since he woke up, which is pretty amazing when you think about what he’s going through.”
“He doesn’t even want to talk about the fire,” Jeremiah adds. “He wants to laugh. He wants to tell jokes. He wants to spend time with his grandkids.”
A Celebratory Ring
On March 5, gibbons was discharged from intensive care at the Burn Center after nearly six months. Still unable to walk (he would take his first tentative steps while in the supportive grip of physical therapists the following week), he emerged from the unit atop a bed being pushed by nurses. A crowd of several dozen friends and family erupted in cheers. Television news crews were on hand as well.
The trip he took that day wasn’t long — he was headed to an inpatient rehab unit in the same building — but it was full of emotional import for family members who had been there or heard about the night that last rites were administered to Pierre Gibbons. By long-standing tradition at the Burn Center, intensive care patients get to ring a celebratory bell upon their release. As Gibbons tackled that task with relish, applause and shouts rang out as well.
Pausing to take questions from reporters, Gibbons deflected their questions about being a hero, telling everyone yet again how that word applies not to him, but to his doctors and caregivers at the Burn Center.
“I’m not a hero,” he said. “I’m a Gibbons.”