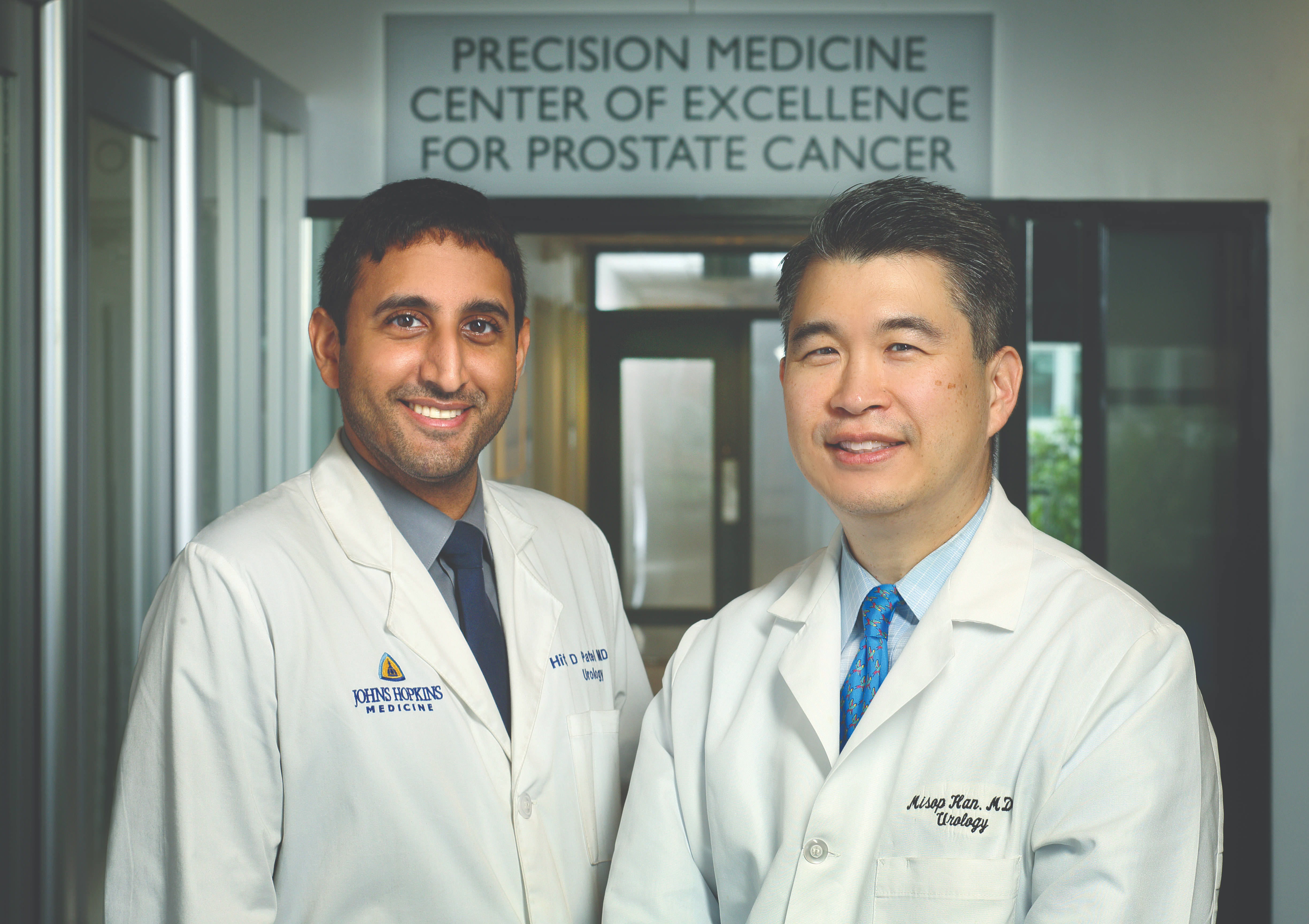
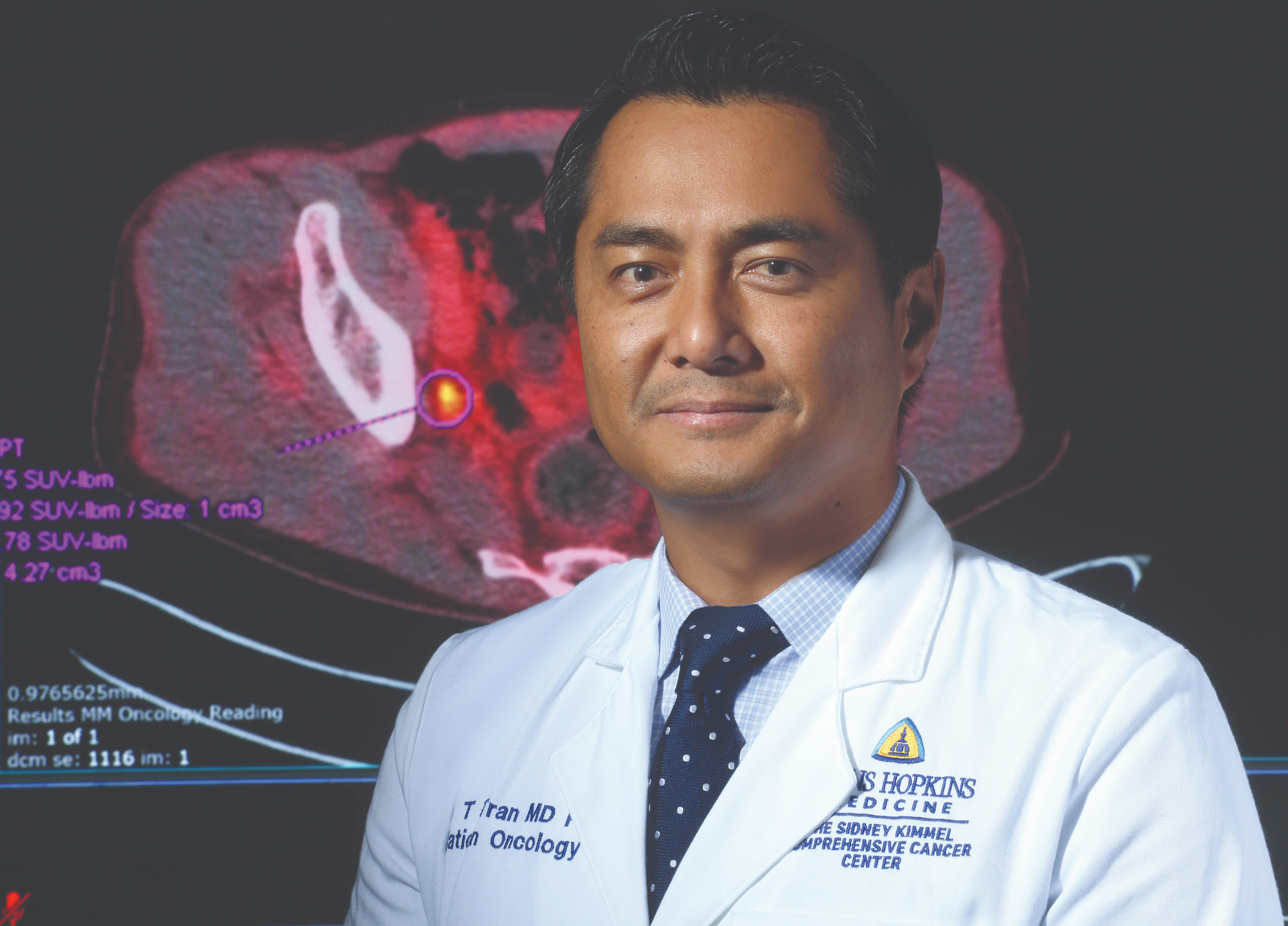
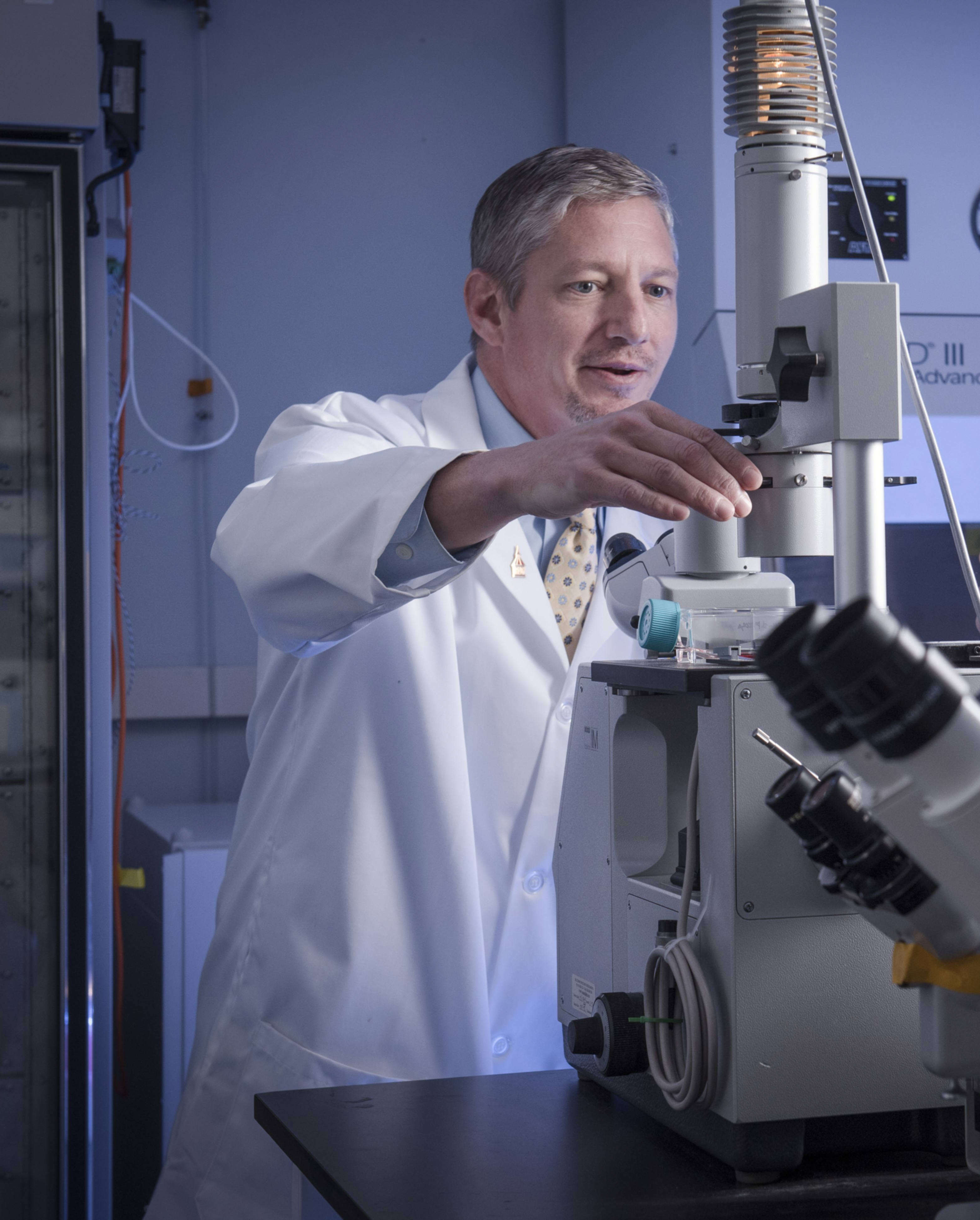
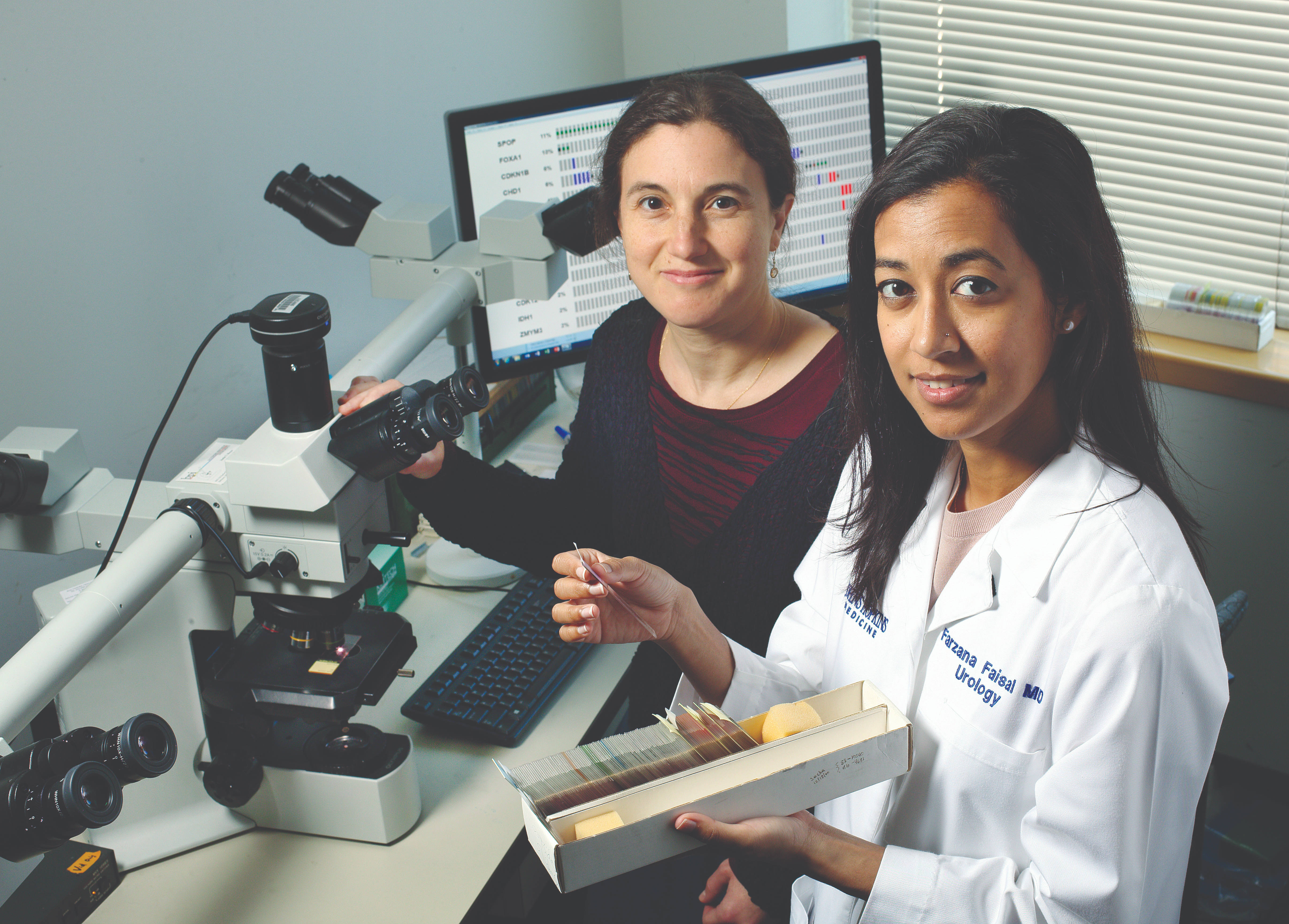
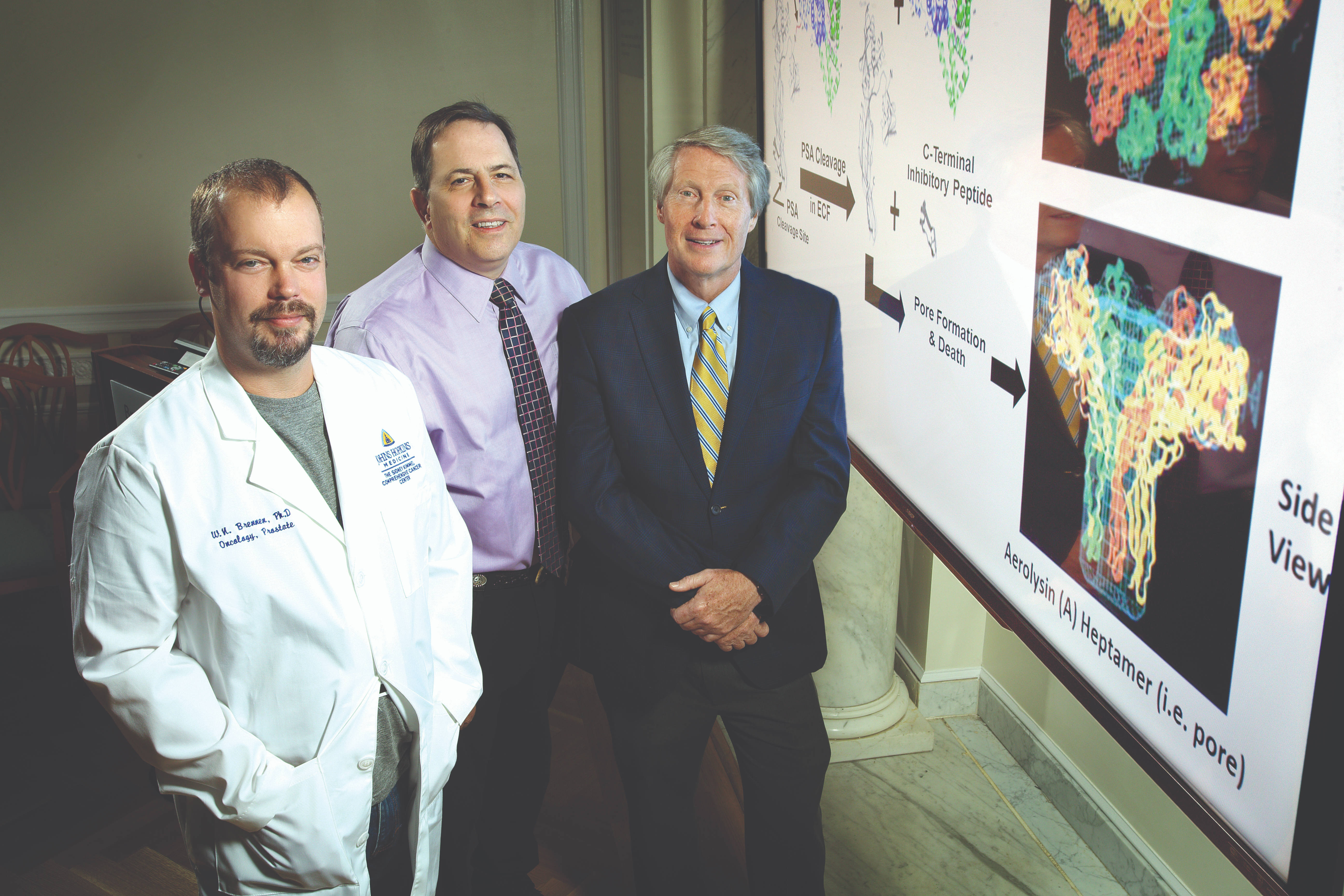
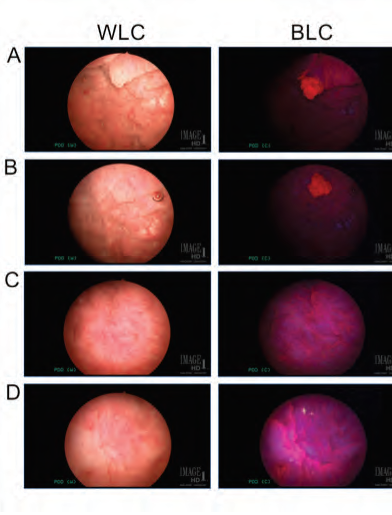
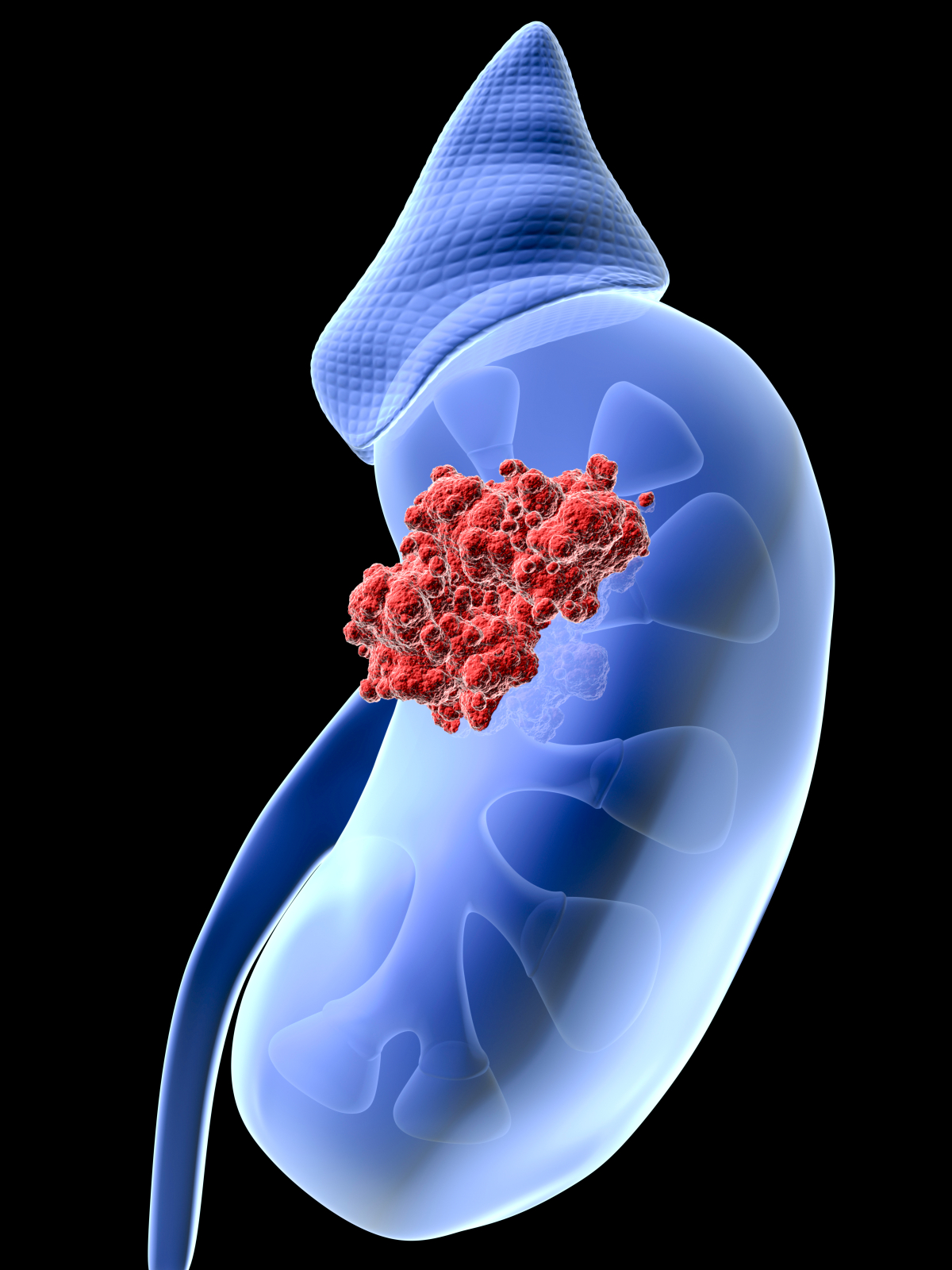
Featured Story Advanced Imaging, Better Biopsy, Smarter Treatment, Fewer Side Effects
Prostate cancer is a curable disease for many patients. In fact, for some men, it requires no treatment at all – but we at the Brady want to make sure we correctly and safely identify those men. For men who do need treatment, we want to address their cancer with few to no side effects.