Labor and Delivery: ‘No One Feels Forgotten’
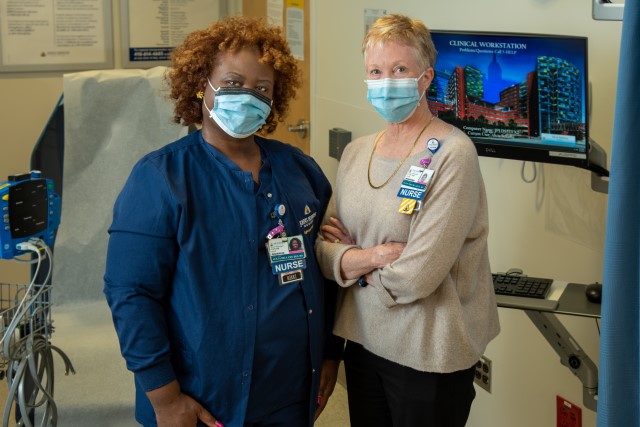
As a staff nurse in the labor and delivery unit on Zayed 8, Nikki Bellamy worried that sick moms and babies were sometimes waiting too long to see a nurse or a doctor.
"When we got especially busy, we had patients sitting in the waiting room as long as eight hours without seeing a medical professional," she says." So we had some near misses, and I just felt we needed a safer practice."
Bellamy shared her concern with obstetrics patient safety nurse Susan Will." And Susan, who is my mentor and hero, said, 'OK, let's get together and brainstorm.'" So, in late 2014 they formed a committee.
"At the time, our triage was first come, first served," says Bellamy." My idea was to provide rooms and care based on acuity, or the urgency of the case. And we wanted the process to be nursing driven."
It took nearly five years of research, trial runs and data collection, but the new system, which includes use of a well-tested obstetrics triage acuity tool, was fully adopted in 2019. Instead of patients checking in with security and registration while an unseen nurse allocates rooms, there is now a dedicated triage nurse who evaluates each patient before registration. That nurse also reevaluates patients at prescribed intervals. Patient wait time dropped 80%, and high-acuity patients are now assigned a room somewhere on the unit even when triage rooms are full.
"It’s been a huge success, and our patients love it because no one feels forgotten," says Bellamy, who was honored this year with the newly created Johns Hopkins Hospital Nurse Professional Practice Model Award." And I learned that as nurses, we can use our voices, not only to take excellent care of our patients, but to effect broader change."
Read more nursing stories in the The Johns Hopkins Hospital 2022 Nursing Annual Report.
