Upper GI Endoscopy
What is an upper GI endoscopy?
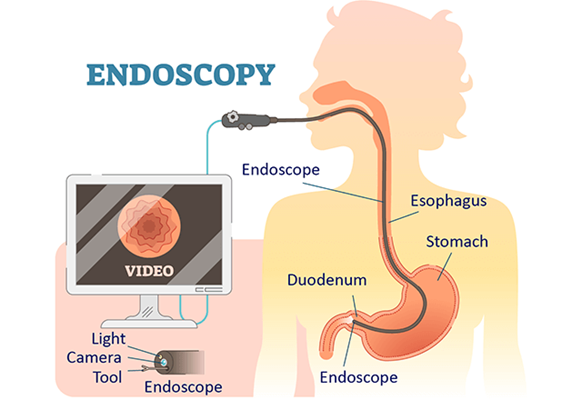
An upper GI endoscopy or EGD (esophagogastroduodenoscopy) is a procedure to diagnose and treat problems in your upper GI (gastrointestinal) tract.
The upper GI tract includes your food pipe (esophagus), stomach, and the first part of your small intestine (the duodenum).
This procedure is done using a long, flexible tube called an endoscope. The tube has a tiny light and video camera on one end. The tube is put into your mouth and throat. Then it is slowly pushed through your esophagus and stomach, and into your duodenum. Video images from the tube are seen on a monitor.
Small tools may also be inserted into the endoscope. These tools can be used to:
- Take tissue samples for a biopsy
- Remove things such as food that may be stuck in the upper GI tract
- Inject air or fluid
- Stop bleeding
- Do procedures such as endoscopic surgery, laser therapy, or open (dilate) a narrowed area
Why might I need an upper GI endoscopy?
An upper GI endoscopy can be used to diagnose and treat problems in your upper GI tract.
It is often used to find the cause of unexplained symptoms such as:
- Trouble swallowing (dysphagia)
- Unexplained weight loss
- Upper belly pain or chest pain that is not heart-related
- Continuous vomiting for an unknown reason (intractable vomiting)
- Bleeding in the upper GI tract
An upper GI endoscopy can be used to identify disorders or problems such as:
- GERD (gastroesophageal reflux disease)
- Narrowing (strictures) or blockages
- Larger than normal veins in your esophagus (esophageal varices)
- Redness and swelling (inflammation) and sores (ulcers)
- Tumors, either cancerous (malignant) or not cancerous (benign)
- The stomach moving upward, either into or next to your esophagus (hiatal hernia)
- Damage caused by swallowing very harmful (caustic) substances, such as household detergents and chemicals
- Celiac disease
- Crohn's disease of the upper GI tract
- Infections of the upper GI tract
An upper GI endoscopy can also treat problems in the upper GI tract. The procedure can be used to:
- Control bleeding
- Remove tumors or growths (polyps)
- Open (dilate) narrowed areas
- Remove things that may be stuck
- Perform laser therapy
- Insert a tube used for tube feeding (a percutaneous gastrostomy tube) into the stomach
- Band abnormal veins in your esophagus (esophageal varices)
An endoscope can be used to take tissue samples (biopsies) or GI fluid samples. An upper GI endoscopy may also be done to check your stomach and duodenum after a surgery.
Your healthcare provider may have other reasons to recommend an upper GI endoscopy.
What are the risks of an upper GI endoscopy?
Some possible complications that may occur with an upper GI endoscopy are:
- Infection
- Bleeding
- A tear in the lining (perforation) of the duodenum, esophagus, or stomach
You may have other risks that are unique to you. Be sure to discuss any concerns with your healthcare provider before the procedure.
How do I get ready for an upper GI endoscopy?
- Your healthcare provider will explain the procedure to you. Ask him or her any questions you have about the procedure.
- You may be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if anything is not clear.
- Tell your healthcare provider if you are sensitive to or allergic to any medicines, latex, tape, and anesthesia medicines (local and general).
- You will be asked not to eat or drink for 8 hours before the test. This usually means no food or drink after midnight. You may be given additional instructions about following a special diet for 1 or 2 days before the procedure.
- Tell your provider if you are pregnant or think you may be pregnant.
- Tell your provider if you have a history of bleeding disorders. Let your provider know if you are taking any blood-thinning medicines, aspirin, ibuprofen, or other medicines that affect blood clotting. You may need to stop taking these medicines before the procedure.
- Your healthcare provider will give you instructions on how to prepare your bowel for the test. You may be asked to take a laxative, an enema, or a rectal laxative suppository. Or you may have to drink a special fluid that helps prepare your bowel.
- If you have a heart valve disease, you may be given disease-fighting medicines (antibiotics) before the test. This may be recommended in certain situations, such as when dilation is being performed. It is not needed for a standard upper endoscopy.
- You will be awake during the procedure, but you will take medicine to relax you (a sedative) before the test. Someone will have to drive you home afterward.
- Follow any other instructions your provider gives you to get ready.
What happens during an upper GI endoscopy?
You may have an upper GI endoscopy as an outpatient or as part of your stay in a hospital. The way the test is done may vary depending on your condition and your healthcare provider's practices.
Generally, an upper GI endoscopy follows this process:
- You will be asked to remove any clothing, jewelry, or other objects that may interfere with the procedure. If you wear false teeth (dentures), you will be asked to remove them until the test is over.
- If you are asked to remove clothing, you will be given a gown to wear.
- An IV (intravenous) line will be started in your arm or hand. A medicine to relax you (a sedative) will be injected into the IV.
- Your heart rate, blood pressure, respiratory rate, and oxygen level will be checked during the procedure.
- You will lie on your left side on the X-ray table with your head bent forward.
- Numbing medicine may be sprayed into the back of your throat. This will stop you from gagging as the tube is passed down your throat into your stomach. The spray may have a bitter taste to it. Holding your breath while your provider sprays your throat may decrease the taste.
- You will not be able to swallow the saliva that may collect in your mouth during the procedure. This happens because the tube is in your throat. The saliva will be suctioned from your mouth from time to time.
- A mouth guard will be placed in your mouth. This will keep you from biting down on the tube. It will also protect your teeth.
- Once your throat is numbed and the sedative has relaxed you, your provider will put the tube in your mouth and throat. He or she will guide the tube down your esophagus, through your stomach, and into your duodenum.
- You may feel some pressure or swelling as the tube moves along. If needed, samples of fluid or tissue can be taken at any time during the test. Other procedures, such as removing a blockage, may be done while the tube is in place.
- After the exam and procedures are done, the tube will be taken out.
What happens after an upper GI endoscopy?
After the procedure, you will be taken to the recovery room to be watched. Once your blood pressure, pulse, and breathing are stable and you are awake and alert, you will be taken to your hospital room. Or you may be discharged to your home. If you are going home, someone must drive you.
You will not be allowed to eat or drink anything until your gag reflex returns. This is to prevent you from choking. You may have a sore throat and pain for a few days when you swallow. This is normal.
You may feel gassy after the procedure.
You may go back to your normal diet and activities, unless you have other instructions.
Call your healthcare provider if you have any of the following:
- Fever or chills
- Redness, swelling, or bleeding or other drainage from the IV site
- Belly pain, nausea, or vomiting
- Black, tarry, or bloody stools
- Trouble swallowing
- Throat or chest pain that gets worse
Your healthcare provider may give you other instructions, depending on your situation.
Next steps
Before you agree to the test or the procedure make sure you know:
- The name of the test or procedure
- The reason you are having the test or procedure
- What results to expect and what they mean
- The risks and benefits of the test or procedure
- What the possible side effects or complications are
- When and where you are to have the test or procedure
- Who will do the test or procedure and what that person’s qualifications are
- What would happen if you did not have the test or procedure
- Any alternative tests or procedures to think about
- When and how will you get the results
- Who to call after the test or procedure if you have questions or problems
- How much will you have to pay for the test or procedure






