The Departments of Neurology and Neurosurgery provide expert care to thousands of adults and children each year, many with rare, complex conditions. Our team of neurologists and neurosurgeons push the boundaries of what's possible through groundbreaking research and clinical trials.
-
Meet Our Experts
Searching for a neurologist or neurosurgeon?
-
Find a Center
Specialty centers, clinics, labs and programs.
-
Patient Stories
Shared experiences from some of our patients.
Request an Appointment
Schedule online through MyChart
Available for follow-up appointments with most clinicians
Log into MyChart
| Sign up for MyChart
Schedule by phone
Adult Neurology: 410-955-9441
Pediatric Neurology: 410-955-4259
Adult Neurosurgery: 410-955-6406
Pediatric Neurosurgery: 410-955-7337
International Patients: +1-410-502-7683
Patient Stories
Skull Reconstruction | Dennis' Story
Nerve Repair | Santi’s Story
Surviving Stroke at a Young Age | Sam’s Story
Hydrogel: The Future of Cancer Treatment
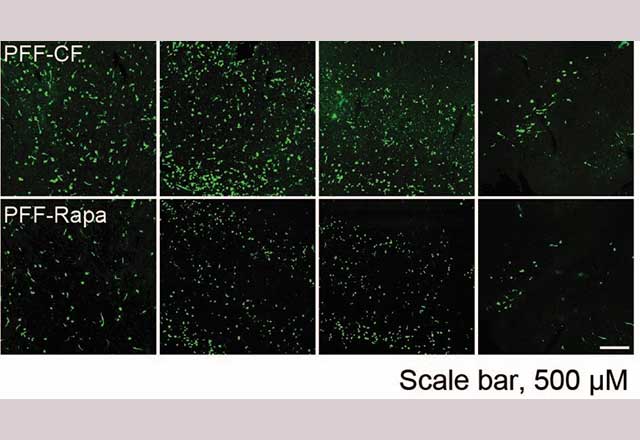
Despite recent technological advancements in the battle against brain cancer, there is a dire need for new treatment strategies. Offering hope in the future of cancer treatment, our team at Johns Hopkins developed a gel to help fend off lingering cancer cells and discourage recurrence after tumor removal.
Read about this researchNews Releases
Charitable Giving
-
Neurology
Support future discoveries by Johns Hopkins neurologists.
-
Neurosurgery
Support surgical advancements and discoveries.