Stereotactic Radiosurgery
What is stereotactic radiosurgery?
Stereotactic radiosurgery is a very precise form of therapeutic radiation that can be used to treat abnormalities in the brain and spine, including cancer, epilepsy, trigeminal neuralgia and arteriovenous malformations.
Stereotactic radiosurgery does not involve an incision or opening; it carefully aims beams of X-rays at abnormal tissues through the skin from multiple directions.
Radiosurgery works in the same manner as other types of therapeutic radiology: The X-ray beams distort or destroy the DNA of cells in abnormal areas so they are unable to reproduce and grow. With optimal treatment, the abnormal tissue becomes inactive and gradually shrinks.
Lesions in the spine or other locations can be treated with a mechanized arm that moves around the patient during treatment.
Reasons for Choosing Stereotactic Radiosurgery
The surgical precision of the technique is particularly useful in treating small or difficult to reach abnormalities in the brain and spine. The targeted focus of the radiation in radiosurgery techniques results in less damage to healthy surrounding tissues and less risk of infection, making it safer for those who have just had surgery.
Possible Side Effects
Stereotactic radiosurgery causes fewer and milder side effects than conventional radiotherapies, which cover a wider area and can affect healthy tissue. The following side effects are typically temporary and get better within a few weeks.
- fatigue
- skin irritation at treatment site
- hair loss at treatment site
- headache
- neurological symptoms, such as seizure, numbness/tingling or weakness
- gastrointestinal symptoms, such as nausea, vomiting or diarrhea
Before the Procedure
Stereotactic radiosurgery takes a team approach, involving specialists in radiation oncology and neurosurgery. A dosimetry expert determines how the beams should be directed and a physicist calculates the amount of radiation the patient should receive, balancing risk and potential effectiveness. A key element of planning the procedure is maximizing the treatment to abnormal tissues, while protecting healthy tissues around the abnormal area.
Together, these experts spend about two weeks planning the procedure. The preparation time may be shorter in the case of an emergency.
During the Procedure
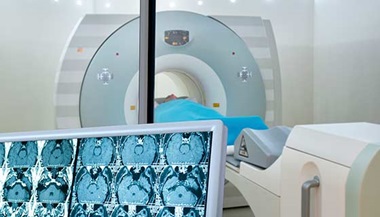
Treatment may take place at an outpatient center. You can expect to spend several hours in the outpatient center, which includes preparation for the procedure, the treatment, and observation after your procedure. You will need to have a friend or family member help take you home. The treatment takes about 30–60 minutes, and you must stay still. There is no incision or cutting. When you arrive, you will meet the treatment team, including doctors, nurses and technicians, who will take care of you. If you are being treated for a lesion in your brain, a head-holder will be placed on your head to keep it totally still. During the treatment, you will be on a hard table, like the table used for MRI or CT scans. Your treatment team will program the machine and deliver the X-rays for your treatment, which include several doses of focused X-rays. After the treatment, you will be moved to a recovery area, where you will be observed to make sure you are feeling well. After you and your treatment team are comfortable, you can go home.
At Home
After treatment, you may resume your normal activities. Your neurology and neurosurgery team will continue to monitor you with CT and MRI during follow-up. Therapy typically only requires one treatment. Some lesions may require more than one treatment session, likely finishing within five treatments. (Conventional radiation therapy can require up to 10 sessions.)