50 Years: In 1974, Patrick and Margaret Walsh Came to the Brady and Transformed It
 Pat and Peg Walsh: Dr. Walsh is looking sharp in the Brady tie — which Peg designed! She based the logo on the Marburg building's cupola, with its double-hung windows that spell "BRADY." The Brady's colors, chosen by Peg from the historic building's red brick and grey grouting, were also used as accent colors throughout the Marburg's interior.
Pat and Peg Walsh: Dr. Walsh is looking sharp in the Brady tie — which Peg designed! She based the logo on the Marburg building's cupola, with its double-hung windows that spell "BRADY." The Brady's colors, chosen by Peg from the historic building's red brick and grey grouting, were also used as accent colors throughout the Marburg's interior.Fifty years ago, Johns Hopkins Medicine made one of its smartest moves ever. When it came time to find a successor for the Director of Urology, venerable William Wallace Scott, M.D., Ph.D., Hopkins had the foresight to hire a young guy, a brilliant surgeon-scientist, fresh out of his 10-year training journey – a rising star who had also been tapped to be the next Chief of Urology at Harvard.*
As the search committee wrote to the School of Medicine’s Advisory Board, Patrick Craig Walsh, M.D., represented “a unique opportunity for bringing into the Johns Hopkins Hospital a young, excellently trained clinician investigator who will be a great stimulus to the future development of the currently outstanding urology program.” And there was a huge bonus: Pat’s wife, Margaret (“Peg”), a gifted interior designer, had wowed the search committee, too. At their recruitment dinner, Dean Russell Morgan said, “I don’t care if Pat accepts the offer, but Peg has to come.” She did, along with Pat and their three young sons.
On July 1, 1974, Walsh, age 36, started work as the third Professor and Director of the James Buchanan Brady Urological Institute, a position he held for thirty years. During his tenure, the Brady became a world-class center for urological patient care, research, and training. At first, though, Pat and Peg had their work cut out for them.
Founded in 1915 by the father of modern urology, Hugh Hampton Young, the Brady had seen better days. The Brady Building itself, along with most of the hospital, had aged without renovation for decades. The full-time faculty in Urology was tiny – just Walsh, Scott, and two junior professors. Within their first ten years, Pat and Peg recruited outstanding faculty and relocated the Brady to the Marburg Building. During this time, Walsh also honed his craft, developing innovative surgical procedures that would transform the field of prostate cancer.
Recruiting Great Faculty
Walsh’s faculty recruits now read like a “Who’s Who” of Urology. He appointed Donald S. Coffey, a first-class scientist and legendary teacher and mentor, as the Director of Research. He also recruited Robert Jeffs from Toronto’s Hospital for Sick Children to head the new Division of Pediatric Urology; and Ray Stutzman, Chief of Surgery at Walter Reed Army Hospital, to become the Director of Urology at Johns Hopkins Bayview Medical Center. He brought in Fray Marshall from Harvard, Michael Droller from Stanford, and Charles Brendler from Duke as specialists in cancers of the kidney, bladder, and prostate, respectively. Also from Harvard, Lou Kavoussi came to develop the new Division of Minimally Invasive Surgery.
Revolutionizing Surgery
The first radical prostatectomy was performed at Hopkins in 1904 by Hugh Hampton Young. But by Walsh’s time, it was rarely performed because of its terrible side effects: impotence, incontinence, and excessive bleeding. Based on anatomical studies, Walsh developed a procedure that created a “bloodless field” – allowing surgeons to see what they were doing! Then, with Dutch urologist Pieter Donker, he discovered the location of the microscopic nerves that controlled erection. On April 26, 1982, Walsh performed the world’s first purposeful nerve-sparing radical prostatectomy and revolutionized the treatment of prostate cancer.
Within a decade, the statistics changed dramatically: in 1982, only 7 percent of men with prostate cancer underwent surgery, but by 1992, with the development of PSA screening to identify more men with curable disease, this safe procedure had become the most common treatment for prostate cancer in the U.S. for men ages 50–70. By 2002, deaths from prostate cancer had declined by 33 percent – greater than seen in any other cancer over the same time period.
This operation also transformed the Brady and Johns Hopkins. Before 1982, fewer than a dozen radical prostatectomies were performed each year. But by 1997, Walsh’s procedure was the most common inpatient operation at the Johns Hopkins Hospital, with over 1,000 cases performed each year. Interest in the procedure grew as urologists from around the world came to watch Walsh and learn his techniques. For years, Walsh worked to make the operation even better, perfecting his surgical technique through meticulous follow-up and analysis of his patients’ outcomes.
Walsh cared deeply for his patients and still does today. He has given every patient his home telephone number. He spoke to all patients he operated on (4,569 men) every three months for the first year following their surgery, and longer as needed. He coached them to recovery, and every year sent them a letter inquiring about their status. He also felt he had a major responsibility to teach urologists how to do this operation well.
He installed excellent video equipment in the operating room so the many visitors who came to watch him operate could see deep into the pelvis.
This turned out to be useful in other ways. Recognizing that small differences in surgical technique could have a major impact on outcomes, Walsh began videotaping his cases, and even spent one summer vacation examining them, stopping the video frame by frame. This enabled him to identify slight variations in technique that significantly enhanced recovery. In 2004, he produced a detailed DVD of the operation, and with generous support from the Mr. and Mrs. Robert C. Baker Family Foundation, he distributed 50,000 copies worldwide free of charge to all urologists who sought one. Today, this video remains a valuable resource for urologists without access to a surgical robot.
Moving the Brady
When Walsh arrived in 1974, the Brady Building had just 13 private beds for patients, and even the single rooms shared a bathroom. Two architectural reviews determined that it would be impossible to renovate the facility for modern inpatient care. The Brady had to be relocated.
Around this time, the Marburg Building – built in 1889– was vacated. With the assistance of William Scott, who raised $2 million dollars, and with Peg overseeing the renovation, this became the Brady’s new home. With more inpatient beds, modern laboratories, a dedicated conference room and library, the space was updated beautifully and thoughtfully. Peg’s elegant design captured the spirit of the historic architecture. The building opened in September 1982, five months after the first nerve-sparing procedure – perfect timing, as patients had started coming to Hopkins from all over the world for radical prostatectomy.
With an abundance of patients, outstanding faculty, and excellent facilities, discovery flourished both in the clinic and in the laboratory. Soon, the Brady was ranked number one by U.S. News & World Report. This also attracted outstanding candidates to the residency program.
Helping Doctors and Patients Worldwide
During Walsh’s 30 years as Director, 62 Urology residents were trained: 87 percent established careers in academic medicine, and 23 became directors of esteemed Urology departments at academic hospitals around the country. But his impact in teaching has grown far beyond the Brady. For 25 years, Walsh was editor-in-chief of the major four-volume, 4,000-page textbook of urology, Campbell’s Urology, nicknamed “the bible of urology,” which was renamed Campbell/Walsh in his honor. For 15 years he served on the editorial board of the New England Journal of Medicine. Together with Janet Worthington, Walsh authored two bestselling books on the prostate and prostate cancer for laypeople. He has authored/coauthored 885 scientific publications. In 2023, Walsh was identified as the most cited urologist in the world, based on the number of influential publications he has authored.
In recent years, Walsh has been invited to give many talks to young physicians about how to make discoveries. He tells them to listen to their patients. If they are asked a difficult question or faced with a challenging fact (like the first patient who told Walsh that he was potent after his radical prostatectomy at a time when this seemed impossible), this is their opportunity for discovery! Also, he advises, learn from Albert Einstein, who said: “The person who follows the crowd will usually go no further than the crowd, but the person who walks alone is likely to find himself in places no one has ever seen before.”
And finally: “Even if they follow all that advice, they will not be successful without the most important ingredient: a partner in life who inspires and embraces their dreams and is willing to accept the sacrifices that will be necessary.” Pat has that partner, and the Brady would not be the same today, had it not been for Peg.
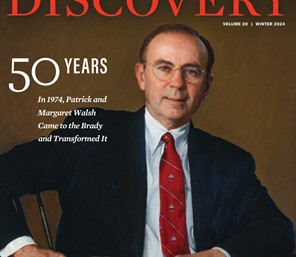 Dr. Patrick Craig Walsh by Peter Egeli, 1998. Image Courtesy of the Alan Mason Chesney Medical Archives.
Dr. Patrick Craig Walsh by Peter Egeli, 1998. Image Courtesy of the Alan Mason Chesney Medical Archives.A fund has been established in celebration of Dr. Walsh’s 50 years at the Brady, to honor his lifetime dedication to surgical advances, education and training, and to support the future of innovation in urologic surgery. For more information, please call 410-955-8434, or contact [email protected].
*Yes, Pat Walsh was supposed to go to Harvard. At age 27, fresh out of his internship at Harvard, he had been told by his mentor, Francis Moore, M.D., the legendary Surgeon-inChief at the Peter Bent Brigham Hospital and the Mosley Professor of Surgery at Harvard Medical School, that he wanted Walsh to be the next Elliot Carr Cutler Professor of Surgery at Harvard and Chief of Urology at the Brigham. Moore then sent Walsh on a nine-year transcontinental training journey that would hone his already impressive surgical skills and provide the opportunity for pioneering molecular endocrinology research. Among other scientific achievements, Walsh was the first to show that cyproterone acetate blocked the stimulatory effect of adrenal androgens on prostate growth. A decade later, this finding was used on a widespread scale in complete androgen blockade of the prostate, and today, powerful antiandrogens have been shown to prolong life in men with advanced prostate cancer.
To Learn More
Celebration of Patrick and Margaret Walsh’s 30 years of contributions to the Brady as of October 30, 2004
www.youtube.com/watch?v=fqWf5h7GoS4
The Brady: 100 years: A History of the James Buchanan Brady Urological Institute at Johns Hopkins
https://jscholarship.library.jhu.edu/items/eedd260b-916b-48cf-9241-73f68dc7505f
Alpha Omega Alpha Leaders in American Medicine: Patrick C. Walsh Interview (1999)
https://www.hopkinsmedicine.org/brady-urology-institute/about-us/history#videos
