Johns Hopkins Radiology Explores the Potential of AI in the Reading Room

Cheng Ting (Tony) Lin in a conference room
Interest in artificial intelligence (AI) has exploded this year as tools such as ChatGPT make AI programs more accessible than ever before. AI has touched nearly every field as researchers begin to look at what the technology can do and how it can improve our lives. Radiology is no exception.
At Johns Hopkins, radiology faculty and operational managers have come together to explore this novel technology through the Radiology Artificial Intelligence Development (RAID) Subcommittee. An offshoot of the Radiology Department’s Value Added Analysis Steering Committee, RAID is chaired by Cheng Ting Lin, an associate professor of radiology specializing in cardiothoracic imaging and a certified imaging informatics professional.
RAID has over a dozen members, including representatives from radiology faculty, departmental administrators, and medical imaging information technology professionals, and regularly consults external groups such as the JHM Data Trust Council, institutional review board and the Johns Hopkins Health System supply chain system.
At each monthly meeting, RAID members discuss the progress of several clinical and research AI projects. The group’s aim is to create a physician-led governance structure to evaluate, prioritize, implement and monitor the use of AI in the radiology department, ranging from investigational algorithms to FDA-approved medical devices.
Artificial intelligence in radiology involves using algorithms to analyze large quantities of data and medical imaging. This has the potential to help radiologists by triaging cases, highlighting abnormalities, and improving diagnostic confidence in the reading room.
Right now, Lin said, medical imaging AI offerings are highly variable in quality, which limits their widespread adoption. Among the chief responsibilities of the RAID subcommittee is evaluating third-party AI algorithms that could, one day, be deployed in our clinical environment.
According to Andrew Menard, executive director of radiology strategy and innovation and a member of the RAID subcommittee, there are currently 400 radiology AI products on the market that are cleared by the Food and Drug Administration, and more are cleared every month. These products focus on different areas, from improving image acquisition to triage, but, as Menard explained, “the most important algorithms are those that make life better for practicing radiologists.”
Radiologists today face ever-increasing volumes and clinical demands, along with diminishing reimbursements. AI technology, he said, “will be a vital component of the Johns Hopkins radiology response to these needs.”
“AI has the potential to automate lower-value work so radiologists can focus on higher-value work,” Menard said, adding, “Implemented properly, this should boost productivity and professional satisfaction while maintaining the quality of radiologic care.”
Lin echoed this sentiment, noting, “AI also has the potential to improve the quality of patient care by adding to radiologists’ confidence in interpretation.”
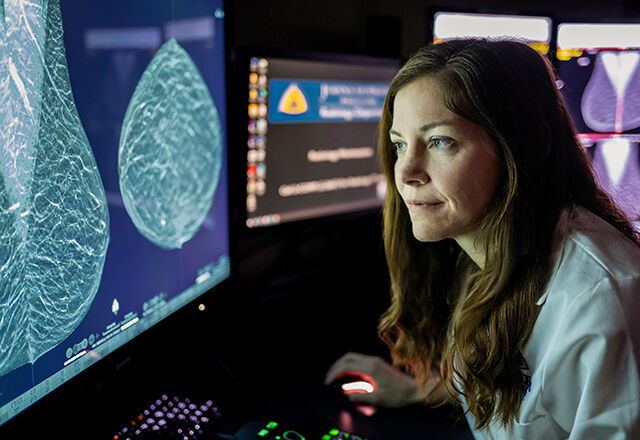 Emily Ambinder in a reading room.
Emily Ambinder in a reading room.
Emily Ambinder, an assistant professor in radiology and radiological science specializing in breast imaging, joined RAID to help figure out how best to incorporate new AI tools into mammography.
She is working with Lisa Mullen, breast imaging fellowship director, who is spearheading RAID’s first physician-led initiative focusing on AI-assisted analysis of screening mammography. Ambinder, Mullein and team have completed an initial evaluation of two leading AI algorithms, and negotiations with the preferred vendor are ongoing.
According to Ambinder, there are many promising FDA-approved AI mammography tools on the market, and many large healthcare organizations are already using AI to analyze mammograms.
While Ambinder understands concerns that AI might “take over” and replace human faculty, she is excited about bringing AI into the reading room. AI is meant to aid radiologists, Ambinder explained, not to replace human intelligence in the reading room.
As such technology is incorporated into routine radiologist workflow, radiologists expect to see both an increase in cancer detection and a decrease in callbacks.
“Envision it as a second set of eyes or a second radiologist looking at the mammogram with you,” Ambinder said.
AI programs do not run autonomously, Ambinder noted. Radiologists will continue to review all cases and findings — AI is just a new tool to aid in detection, diagnosis and triage.
“We are looking for tools to increase the value of radiologists, not replace them,” Lin explained.
That said, there are some limitations to current AI technology.
Third-party algorithms from outside of Johns Hopkins may not be as accurate, Dr. Lin said, noting that such programs were trained using patient data with different demographics and characteristics from those who seek care at Johns Hopkins. As such, the algorithm may not perform as well once implemented and require ongoing monitoring.
However, as home-grown, in-house AI tools are developed, such issues can likely be overcome.
For Lin, the future of AI in the radiology reading room looks bright. He foresees Johns Hopkins one day becoming a premiere institution of artificial intelligence that uses such machine-learning programs to identify conditions and potential treatments faster and more accurately.
An equally important goal, Dr. Lin explained, is to support internally-developed algorithms and work with experts at Johns Hopkins to bring their AI tools from bench to bedside.
One effort to expand the use of AI in medical imaging analysis is RAIL (Radiology AI Lab), a partnership among the Johns Hopkins radiology department, the Malone Center for Engineering in Healthcare, the Applied Physics Laboratory and the Whiting School of Engineering.
Headed by Haris Sair, director of the division of neuroradiology, RAIL works with departments across Johns Hopkins to develop machine learning applications to better aid medical image classification and analysis.
However, just as Rome wasn’t built in a day, so too does building an AI program take time.
As Lin noted, it is imperative to have a robust governance structure in place, allowing methodical development, piloting and evaluation of AI tools across the department and system.
“There are no shortcuts for this process,” Lin said.
Lin envisions a future when, due to assisted analysis, detection and diagnosis, more lives are saved than ever before.
