The Transplant Experience
The staff at the Johns Hopkins Comprehensive Transplant Center will be with you every step of the way, telling you what to expect next, and how to prepare for your experience.
As you come into the transplant program at Johns Hopkins, you probably have many questions: How long before I can have a transplant? What kind of tests will you run on me? Where can I find support during this time?
Before Your Transplant
There are several steps and considerations to make before your transplant:
Referrals
There are two ways to be referred to the Johns Hopkins Comprehensive Transplant Center - physician driven referral or self referral. Your physician specialist may refer you directly to the transplant program. We ask that your specialist forward your medical records including demographics and insurance information. Once this information is reviewed a member of the transplant team will contact you regarding appointment scheduling.
The second way to come to the Comprehensive Transplant Center is to self-refer. Self-refer means that you call the transplant program directly and ask us to send you the referral information packet. This packet contains the candidate form and informed consent document. It is important to return the candidate form, along with photocopies of your insurance cards, to the transplant center within two weeks. The informed consent document is provided for your information and will be discussed in great length at your evaluation appointment.
-
Heart Transplant
-
Kidney / Pancreas Transplant
-
Liver Transplant
-
Lung Transplant
Kidney Transplant Referral Frequently Asked Questions
-
For most individuals, a nephrologist or primary care provider will advise you on when kidney transplantation is the best course of action. This care plan is put in motion when an individual is diagnosed with a condition that results in End Stage Renal Disease (ESRD).
-
In order to receive a kidney transplant at Johns Hopkins you must have adequate health insurance. Prior to being evaluated for transplantation, all patients will have their insurance verified by the transplant financial advocates. This process informs you and the transplant center of your insurance benefits related to transplantation and whether The Johns Hopkins Hospital is in network and accepts these benefits.
If The Johns Hopkins Hospital is out of network or your insurance company does not work with/contract with Johns Hopkins, the transplant financial advocates will work with you to inform you of transplant centers who are in network.
Lung Transplant Referral Frequently Asked Questions
-
For most individuals, a Pulmonologist or Primary Care Provider will advise when you should be referred to a transplant center for consultation. Often, they will refer for a second opinion and to determine whether a lung transplant is an appropriate treatment option. Usually, a referral is made for individuals with end-stage, non-malignant types of lung disease where transplant would either be life saving or a live-improving measure. The most common diseases for lung transplant referral are: Chronic Obstructive Pulmonary Disease (COPD), Pulmonary Fibrosis, Pulmonary Artery Hypertension and Cystic Fibrosis (CF). Lung transplant is considered the ultimate treatment after all other medical therapies have been exhausted and the lung disease poses significant impact on quality of life and/or a person’s survival.
-
In order to receive a lung transplant at Johns Hopkins you must have adequate health insurance. Prior to being evaluated for transplantation, all patients will have their insurance verified by the transplant financial advocates. This process informs you and the transplant center of your insurance benefits related to transplantation and whether The Johns Hopkins Hospital is in network and accepts these benefits.
If The Johns Hopkins Hospital is out of network or your insurance company does not work with/contract with Hopkins, the transplant financial advocates will work with you to inform you of transplant centers who are in network.
Your Transplant Evaluation
All patients will receive an initial evaluation by members of the transplant team. Some patients will move immediately toward being listed for transplantation, while others will be able to manage their condition for months or years before transplantation becomes necessary. Only after the evaluation is complete can the transplant team tell if a patient is eligible for a transplant.
Prior to your first appointment, you'll be asked for provide a list of all prescription, over-the-counter and herbal medications, including name, dosage and frequency of use. You'll also be asked for a copy of your medical history and any recent test results. If you are unable to send the requested information ahead of time, please bring this with you the day of the appointment.
Once all tests are completed, the transplant team will review your case and determine your transplant eligibility.
Evaluation Tests
Patients may require additional medical testing, which may result in follow-up visits to the hospital. Some candidates may be able to have these test performed in their local area. Patients can take an active role in moving the evaluation testing along by following through on completing the tests that are needed.
Depending on a patient’s situation and type of organ transplant, the following tests may or may not be required:
-
- Cancer Screening – For those with a history of cancer, certain medical testing may be required to determine transplant eligibility.
- Abdominal CT Scan – This test shows the size and shape of your abdominal organs and main blood vessels.
- Chest X-ray – Looks for infection or fluid in the lungs.
- Blood Work – Transplant specific blood work will be required for all potential transplant recipients. This will be explained during your evaluation appointment.
-
- Pulmonary Function Tests – Tells how well your lungs are working.
- Electrocardiogram (EKG) – Reveals your heart rhythm.
- Stress Echocardiogram – Shows the size and function of your heart, checking to see how the blood flows through your heart, and sees if any areas are not receiving enough oxygen.
- Liver Biopsy – Removes a small piece of liver for analysis.
-
- Substance Abuse – Active substance abusers will not qualify for a transplant. Typically, at least six months of documented sobriety or abstinence is required. If a patient is approved for transplant, random checks may be performed to ensure sobriety.
- HIV – Patients with HIV may still be eligible for a transplant. Other criteria must be met.
- Smoking – It is recommended that you stop smoking. Smoking may increase the amount of time you spend on a ventilator post transplant, and could cause slower wound healing.
Organ Donors
There are two types of organ donors, deceased or living. Deceased donor organs are obtained through procurement services offered by the Living Legacy Foundation of Maryland (LLF), a non-profit organ and tissue donation program.
The Johns Hopkins Comprehensive Transplant Center encourages live organ donation for our kidney transplant patients. We also offer a live donor program for liver transplant patients as well.
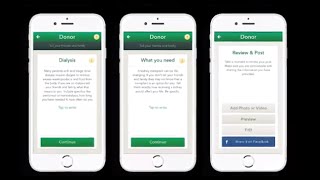
#TomorrowsDiscoveries: Using Technology to find Organ Donors– Andrew Cameron, M.D., Ph.D.
Andrew Cameron, a liver transplant surgeon, recognizes that many people wait on the transplant list. He and his team worked with Facebook to allow people to show their friends they are registered organ donors. The initiative tremendously increased donor registration rates. Dr. Cameron’s team is now working on an app to help patients identify a living donor.
Benefits of Living Donation
There are many benefits to having a living donor. Often, a living donor is a relative. Such genetic matches lower the risk of organ, and genetically matched organs actually begin to function sooner than non-genetically matched organs.
Having a living donor also shortens the amount of time a patient spends on the waiting list. Furthermore, living donation surgeries can be scheduled, allowing for the patient and the donor to find a time that works best (summer vacation, winter break, etc.)
Find out more about live organ donation.
The Waiting List
The United Network of Organ Sharing (UNOS) manages the waiting list for organ donation. UNOS is a federally-contracted, non-profit organization that matches donors to recipients and ensures that organ allocation policies are followed.
Thousands of people are currently on the organ waiting list. A person’s position on the list depends on a number of factors, based on the needed organ. The transplant team at Johns Hopkins will help you understand the waiting list in relation to your transplant.
-
The sickest patients get priority on the heart transplant waiting list. Factors include length of time on the list, organ match (blood type and body size), and the geographic distance of the deceased donor to the transplant center.
-
Patients who do not have a living donor rely on the waiting list to secure a new kidney and/or pancreas. A person’s position on the waiting list for a kidney and/or pancreas can be affected by his or her length of time on the wait list and a blood type and antigen match to available organ.
-
Wait time for a liver depends on a patient’s MELD (Model for End-stage Liver Disease) or PELD (Pediatric End-stage Liver Disease) score. These scores range from 6 (less ill) to 40 (gravely ill), and are based on routine lab test results: bilirubin, which measures liver damage; creatinine, which measures kidney function, sodium; and INR, which evaluates clotting. The average wait time varies based upon blood type and severity of illness.
-
Patients are assigned a Lung Allocation Score (LAS), based on lung function, pulmonary artery pressure, oxygen needs, pulmonary capillary wedge pressure, and other general conditions. LAS range from 0 (less ill) to 100 (gravely ill). Scores are updated every six months based on regularly scheduled testing, or at any point if a patient’s clinical status changes.
Receiving the Call
Unless your transplant is scheduled, when a donor organ becomes available, you will receive a phone call. This can occur at any time. When you get the phone call, you should proceed to the designated location to prepare for surgery.
It is important to know that false alarms do occur. Due to time constraints, an organ may not be fully evaluated before you come to the hospital. When all the information is available, your surgeons will know whether or not it is the right organ for you. While false alarms can be frustrating for transplant patients and their families, it helps to ensure that the best organ is found.
During Your Transplant
When you arrive at the hospital, your blood will be drawn and you’ll receive a physical exam. You may need an X-ray or an EKG. You may be asked to scrub yourself clean. Finally, you will be anesthetized for the surgery.
-
Auto Islet transplant surgery lasts approximately eight to ten hours. Patients may stay in the hospital for 10-14 days after surgery.
-
Hand transplant surgery is extensive. Patients may stay in the hospital for several days and will experience months of intense physical therapy.
-
Kidney and Pancreas transplant surgery takes approximately four hours, depending on a patient’s medical condition and previous surgeries. Patients stay in the hospital for approximately seven days after an uncomplicated surgery. For a simultaneous kidney/pancreas transplant, the average stay is 14 days.
-
Liver transplant surgery lasts anywhere from six to twelve hours. After an uncomplicated procedure, the average hospital stay is seven days.
-
Heart transplant surgery takes approximately six hours to perform. Typically, the length of hospital stay after a heart transplant is seven to ten days.
-
Lung transplant surgery lasts approximately six hours. The average hospital stay after a lung transplant is seven to fourteen days.
After Your Transplant
Recovery and rehabilitation should be your main concerns after your transplant. Your transplant team, including surgeons, specialists, nurses, dieticians, and social workers will follow you throughout your recovery. Each patient’s path to recovery is different, and it can be months before a patient is fully healed from the surgery.
Following your recovery plan is essential for healing. After your surgery, you’ll spend several days in the Surgical Intensive Care Unit (SICU). You will have many monitors attached to you to keep track of your condition:
- Nasogastric Tube (NG Tube) – This tube is placed through your nose and down into your stomach to keep your stomach clear. It will be removed when your bowel function returns and you are able to eat. It may make your nose and throat sore.
- Endotracheal Tube (breathing tube) – This tube will remain in place until you are awake enough to breathe on your own. It is usually in place for one to two days after surgery. While this is in, you will not be able to talk. Your family may want to bring pen and paper so that you can express yourself. You may also want to establish simple movements, such as blinking, for yes or no questions.
- Urinary Catheter (Foley) – This tube helps empty your bladder. It is removed once you are more awake.
- Central IV Lines – These lines help provide fluids, nutrition and medication. They are removed when you can eat and drink. You and your caregiver will be instructed in how to manage your care during your recovery period. This includes medication information and daily living instructions.
After your transplant, you will have regular appointments in an outpatient clinic. As you improve, these appointments will be less frequent. Arrangements for blood tests and medication management can be made through your primary care provider, or through your local Johns Hopkins Community Physician.
The United Network for Organ Sharing requires that hospitals follow-up with patients for at least two years after a transplant. Often, the relationships developed between our physicians and patients last decades longer.