Illustraton by Michael Glenwood
Could advances surrounding a newly discovered “X cell” hold the clue to preventing type 1 diabetes from taking hold in the first place? That’s the hope of a team of Johns Hopkins scientists whose arduous bench-side journey might be close to paying off.
The conversation never gets easy, Thomas Donner says, no matter how many times you’ve done it: It’s always painful to tell a patient that they’ve developed type 1 diabetes, an incurable autoimmune disease that will require lifelong insulin therapy and a constant awareness of their glucose levels. For these patients, who are typically 10 to 13 years old but can be any age at the time of diagnosis, no decision about what to eat, what to drink or how to exercise will ever be simple again.
“These patients basically need to be thinking about their diabetes all day long,” says Donner, an associate professor of medicine who directs the Johns Hopkins Diabetes Center. “It’s a very demanding disease.” If they allow their glucose levels to run chronically high, they risk irreversible damage to their eyes, kidneys and cardiovascular system; if glucose drops too low, they can suffer seizures or coma.
But now, thanks to a remarkable series of studies at Johns Hopkins, Donner sees reason to hope that there will be fewer of those conversations in the future. Within a decade, Donner says, there may be a treatment that would prevent type 1 diabetes from developing in the first place.
Ten years ago, Donner was approached by Abdel-Rahim Hamad, who directs an immunology laboratory at Johns Hopkins. Hamad had begun his career by hunting for immune cells that might be useful in treating cancer. Along the way, he’d spotted an interesting pattern in the lab: Certain genetically modified mice in his cancer studies seemed somehow to be protected against autoimmune diseases. He asked Donner if he’d be interested in exploring the implications for type 1 diabetes.
Last year, their collaboration paid off dramatically. In a paper in the journal Cell, Hamad, Donner and their colleagues reported extraordinary discoveries about the machinery that drives type 1 diabetes — and possibly other autoimmune disorders. Hamad’s lab has identified a previously unknown type of lymphocyte that combines features of both B cells and T cells. In people with type 1 diabetes, this hybrid lymphocyte — which Hamad has dubbed the X cell — carries a peptide that primes the immune system to attack insulin-producing cells.
This discovery has shed new light on the long-standing mystery at the heart of type 1 diabetes: Why and how exactly does the immune system decide to attack and destroy the insulin-producing islet cells in the pancreas?
And with that new understanding, Donner says, the discovery of the X cell has opened up new possibilities for preventing and treating type 1 diabetes. Before long, he hopes, he and colleagues will manufacture an antibody that targets and inactivates or destroys the X cell. If all goes well, this new therapy might protect at-risk people before symptoms ever emerge.
“When I first started med school in the 1980s, there was a perception that people with type 1 diabetes would have significantly shortened life spans,” says Donner. “That perception has changed dramatically, but it’s still a very difficult disease to manage. What we’d really like to do is stop it from developing in the first place.”
“I’m very lucky,” says Laurie Hart, a diabetes advocate who has been a patient of Donner’s for three years and who has donated funds to support his research. “I’ve had type 1 diabetes for 41 years with relatively few complications. But I hear every day from people who are struggling with complications and struggling to afford insulin. If Dr. Hamad and Dr. Donner’s research helps us identify children at risk of type 1 diabetes and prevent the disease from developing, that would be life-changing for so many people.”
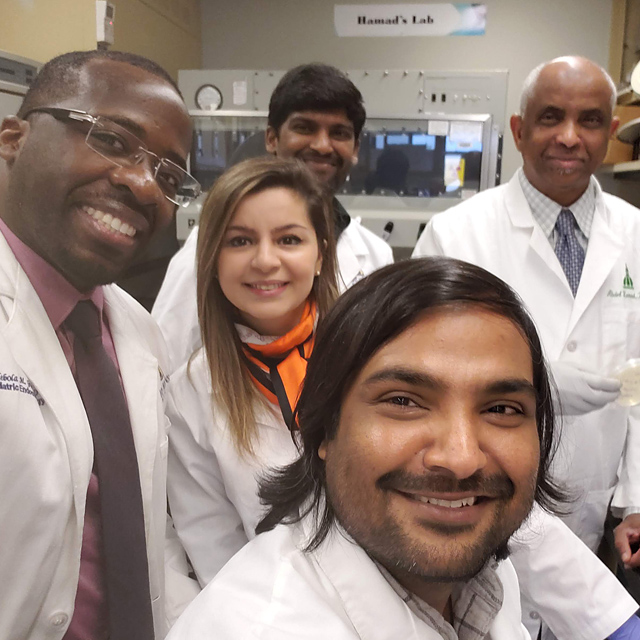
Clockwise from center, front: Rizwan Ahmed, Adebola Giwa, Abdel-Rahim Hamad, Mohan Sadasivam, Zahra Omidian (center).
‘Extraordinary Evidence’
The seeds of this research were planted in the late 1990s, when Hamad arrived from his native Sudan to take a postdoctoral position at Johns Hopkins. He was assigned to the laboratory of Drew Pardoll, a pioneering researcher in immunotherapies for cancer. In Pardoll’s lab, Hamad studied a variety of rare and unconventional immune cells, in an effort to see if they might be weaponized against cancer. As he worked with genetically modified mice in Pardoll’s lab, Hamad occasionally came across cells that seemed to express both B cell receptors and T cell receptors. Those cells had been previously noticed by other researchers, but they’d generally been shrugged off as “doublets” — that is, pairs of T cells and B cells that happened to cling together, not true hybrid immune cells with single nuclei.
“People just ignored them,” Hamad says. “They called them abnormal lymphocytes. But I never bought that. I always thought that they must have a real function. I put the problem on the back burner for many years, but I never forgot about it.”
In 2015, in the course of his collaboration with Donner, Hamad finally got his chance to focus on the problem. With the help of a $50,000 grant from the Johns Hopkins Discovery Award program, Hamad and his postdocs started to search seriously for these hybrid cells.
“In the early phase of this research,” Hamad says, “some people were so skeptical. The nicest people would just sort of look at you and change the subject. But I understand. To tell people that there is a cell that is a hybrid between a B cell and a T cell is a tall order. For an extraordinary discovery, you need extraordinary evidence.”
The first challenge that Hamad’s team faced was that the X cells comprise only a tiny fraction of a person’s immune cells. “If I started with a pool of 60 million to 80 million lymphocytes, I might eventually find 1,000 of these X cells,” says Rizwan Ahmed, a postdoctoral researcher in Hamad’s lab. “It’s very discouraging work. It would take me hours and hours to use flow cytometry to separate those cells.”
That laborious census of the X cells soon paid off: In collaboration with Hao Zhang, a research associate in the lab, Ahmed confirmed Hamad’s hunch that the population of X cells would be elevated — still tiny, but elevated — in people with type 1 diabetes.
“If these cells were just doublets,” Ahmed says, “they should have had a more or less random frequency. But in people with type 1 diabetes, they had a very consistent frequency. So that was when we thought that these must not be doublets, that these are real cells with a real function.”
The team decided to send a blood specimen from a patient with type 1 diabetes to Adaptive Biotechnologies, a Seattle firm that performs genetic sequencing. “They called me and said these cells are very interesting,” Hamad says, “because they have B cell receptors and T cell receptors, but the B cell receptors all seem to be a single clone.” Six months later, Hamad’s lab sent a specimen from a different patient with type 1 diabetes: It turned out to have the same clone. A few months later, a third patient: the same clone.
“To find the same 16-amino-acid sequence on cells from three of my patients with type 1 diabetes — the chances of that are millions to one,” Donner says. “And then we looked more closely at that 16-amino-acid sequence and saw that it had a lot of structural similarities to insulin.”
Here, Donner and Hamad knew, might lie answers to some of the most vexing questions about type 1 diabetes: What exactly triggers the autoimmune syndrome in the first place? Why does the body decide to attack its own pancreas?
A Sequence with Answers
Decades ago, researchers thought that insulin itself might be the antigen that stimulates the autoimmune response. But that turned out to be wrong: In people with type 1 diabetes, insulin typically stimulates a modest autoimmune reaction, but not one strong enough to account for full-blown attacks on their islet cells.
More recently, scientists have been fixated on the fact that people who inherit certain variants of the HLA-DQ antigen — one of the molecules responsible for helping the immune system distinguish between “self” and “not-self” — are at high risk of developing type 1 diabetes. But that explanation seemed incomplete: Why do only a small fraction of people with the troublesome HLA-DQ variants actually develop type 1 diabetes? And when it does happen, exactly which cells are the HLA-DQ antigen interacting with? Scientists couldn’t tell.
The 16-amino-acid sequence on these X cells — which Hamad’s team has termed the x-idiotype peptide — offers some answers. When Hamad’s lab exposed autoimmune cells to this peptide, the cells reacted 10,000 times more strongly than they do to simple insulin. They released huge volumes of cytokines and recruited other immune cells to attack. Here at last was an autoimmune process strong enough to explain the destruction of a person’s islet cells.
“Next, we wanted to see exactly why this peptide sets off such a strong reaction,” Ahmed says. “We collaborated with Ruhong Zhou at Columbia University, who did molecular simulations for us. He found that this peptide has a perfect binding register for the high-risk version of the HLA-DQ molecule. In other words, they attach to each other very strongly.” A second mystery was solved: Now it is clearer why people who inherit the high-risk versions of the HLA-DQ antigen can easily fall prey to type 1 diabetes.
Many questions remain. For one, many people who inherit the high-risk variants of HLA-DQ never actually develop type 1 diabetes. Why not? What exactly drives the onset of disease? For decades, scientists have suspected that acute viral illnesses can act as triggers for type 1 diabetes and other autoimmune conditions. The onset of type 1 diabetes appears to be more common in the winter, when viral infections are prevalent, and patients often recall having had the flu a few weeks before their diabetes symptoms began.
“We don’t have any new evidence about this yet,” Ahmed says. “I can only speculate. But one thing you can imagine is that viruses somehow integrate their DNA within the X cells so that they can evade the immune system.” Or it may simply be that the body’s immune response to the flu causes a temporary increase in the number of circulating X cells. For most people, that’s no problem. But in people who have inherited the high-risk versions of the HLA-DQ antigen, the strong binding between the X cells and the HLA-DQ antigen sets off a cascade of autoimmune processes that ends with the destruction of the pancreas’ islet cells.
Preventing Diabetes in the First Place
Now that the X cell has shone new light on the immune mechanisms that underlie type 1 diabetes, are we any closer to a cure?
Donner is cautious about speculating about cures for people who have already developed type 1 diabetes. But he and his colleagues have high hopes that their discoveries might lead to treatments that would protect at-risk children from developing the disease in the first place.
“We have a very strong suspicion that these X cells are detectable before the actual onset of the disease,” says Adebola Giwa, a pediatric endocrinologist who divides his time between clinical care and bench science in Hamad’s lab.
“And if that’s the case,” Donner adds, “we could potentially knock this cell out even before there’s been any destruction of the pancreas.”
Here is how it might work: At a young age, every child could be screened for the presence of diabetes-related X cells — that is, those that carry the x-idiotype peptide. Children who screen positive on that test could be given an injection of monoclonal antibodies that specifically target that peptide.
“This 16-amino-acid sequence is not found in any other cell in the human body,” Donner says. “Which is great. That means that we should be able to create an antibody to it without worrying about other cellular damage.”
Hamad’s lab has already begun to work on crafting such an antibody — using mouse models, so far. They expect to create a humanized version of such an antibody within a year.
To begin this antibody research, the lab had to establish a sustainable, immortalized line of X cells. That task fell to Zahra Omidian, a postdoctoral researcher who joined Hamad’s lab in 2017. “It was a very, very challenging process,” she says. “It really took a year to get the process right.” Compared to the initial arduous process of cloning the cell line, Omidian says, the process of developing antibodies to target the X cell should be a bit easier.
Unfortunately, Donner says, an antibody to prevent type 1 diabetes may not be a one-time treatment. People at risk of the disease would probably require antibody infusions periodically, much as patients with rheumatoid arthritis (another autoimmune condition) receive antibody infusions on a monthly basis.
Would antibody therapy do any good for people who have already developed full-blown type 1 diabetes? Donner says it’s possible. That is because even in full-blown disease, most type 1 patients show evidence of functioning islet cells. “Even in patients whose disease onset was quite a while ago,” he says, “we can measure a substance called C-peptide that is only released by islet cells. It is possible that pancreatic stem cells mature into islet cells that survive a short time before undergoing autoimmune attack.” If antibody therapy can shut down the autoimmune attacks, he says, such regenerating cells might be able to effectively produce insulin again.
“These patients might still require insulin injections,” Donner says. “But it might be a much smaller amount than they require today and would make the management of their disease considerably easier.”
All of these therapies are still theoretical, but Donner and his colleagues are hopeful that they can bring them to fruition. “My patients and their parents just light up when I ask them if they’d be willing to donate blood specimens for this research,” Giwa says. “Diabetes is not easy to live with. When I tell parents that there’s a chance they could help prevent this from happening to other kids — and conceivably even help their own child — they’re really happy to participate.”
Implications for Other Autoimmune Diseases
The excitement around the discovery of the X cell goes well beyond type 1 diabetes. Hamad believes that the cellular mechanisms his lab has discovered might be involved in other autoimmune disorders. Last summer, the lab received a $3 million grant from the W. M. Keck Foundation to broaden its studies of the X cells. Already, Hamad and his colleagues have looked at Graves’ disease and multiple sclerosis.
“At this point, I’m confident that peptide clones like the one we found for type 1 diabetes are also present for all organ-specific autoimmune diseases,” Hamad says. “And we’re starting to look at systemic autoimmune diseases, like lupus.”
The strange hybrid form of the X cell, Hamad says, makes it an especially potent force in autoimmune disease. “Normally, T and B cells need to interact with each other to activate each other,” he says. “But it appears that the X cell can sometimes essentially activate itself. It doesn’t need any other collaborator. And that’s what makes it dangerous. X cells have all the elements — they can just interact with each other without having to interact with an antigen-presenting cell or another T cell.”
Donner says that this kind of novel discovery is exactly the kind of ambitious research he hoped to do when he joined Johns Hopkins in 2010. “Type 1 diabetes can cause very, very serious complications,” he says. “If we can help lift that disease burden, that will be a great achievement.”