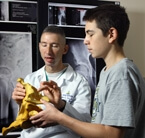
Explaining hip arthroscopy, pediatric orthopedic surgeon John Tis with patient Kieran Carroll.
Gaithersburg, Md., patient Kieran Carroll, 15, started feeling pain in his left hip in July 2009 during a game of soccer. The pain got worse and orthopedists in the Washington, D.C., area told him he had tears in his labrum – the cartilage that rims the socket, or acetabulum, of the hip joint – which they could repair in an open surgery. What they couldn’t do, however, was resolve the underlying anatomical and biomechanical causes of the tears. That’s when he came to orthopedist John Tis.
“Is there too little bone or too much bone in the hip?” Tis says. “What is the underlying cause of the cartilage damage and labral tears? Why is someone only 15 years old with no specific injury having these tears?”
Tis explains that for decades orthopedic surgeons couldn’t figure out why relatively young patients like Carroll had 1abral tears yet no trauma and no apparent cause. Answers started to come in the 1980s when German orthopedic surgeon Reinhold Ganz performed a series of operations to provide patients’ hip sockets with more “coverage” of the femoral ball. He learned that not only could children not have enough coverage, resulting in the hip falling out of the socket, but they could have too much coverage, resulting in too much friction, and what Ganz coined femoroacetabular impingement, or FAI.
“If you have too much coverage the cup constrains the ball too much, or the ball is not perfectly round and bumps up against or impinges the cup,” Tis says. “Either way, the condition predisposes you to arthritis.”
Part of the problem, Tis says, is that MRI and other diagnostic imaging may reveal a rip in the labrum but not underlying culprits like FAI. Neither do open surgical incisions lend themselves to good visualization of the hip. So Tis uses minimally invasive hip arthroscopy, feeding a pencil-sized fiber optic scope through a tiny incision to explore the hip. Not only can he clearly see what diagnostic imaging doesn’t show, but using the same tools he can fix the problem by contouring the hip and removing bony fragments impinging the hip, reducing the risk of tears recurring.
“The advantages include less scarring and stiffness, and a faster recovery,” Tis says. “Instead of three days in the hospital, it’s same-day surgery and you’re up and walking the next day.”
Kieran, it turns out, had FAI in both hips, which Tis treated in two minimally invasive procedures. “Kieran’s response has been really good,” says his father, Dan. “He has a lot more flexibility and no pain.”
For more information or to schedule an appointment call (410) 955-9444.
