Walking was uncomfortable. Sitting was uncomfortable. Exercise was OK, but not jumping.
For 85-year-old Joan Kravets, vaginal prolapse was a constant nuisance. The condition happens when the muscles that support the pelvis weaken and other organs bulge or fall into the vagina. Symptoms include vaginal discomfort that can feel like pressure or throbbing pain, and impairments to bladder or bowel function.
“To walk or to do anything, it was just very uncomfortable,” the Northern Virginia resident says.
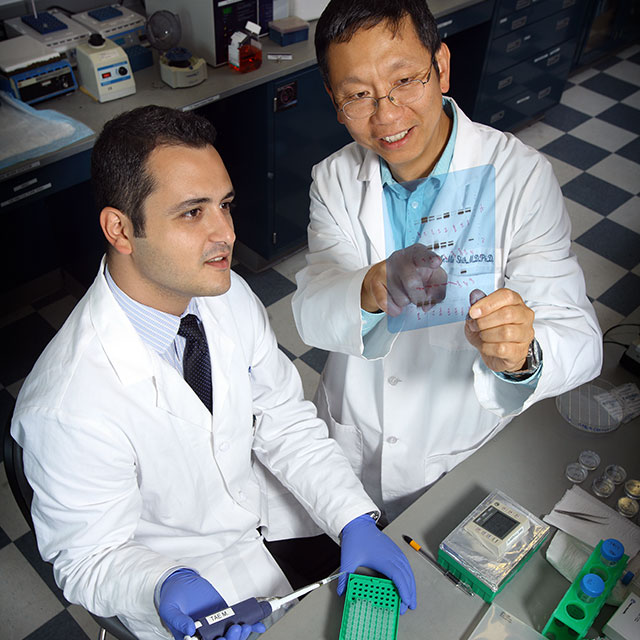
After searching for the right doctor, Kravets chose urogynecologist Daniel Gruber, drawn in by his approachable demeanor. Gruber is director of Sibley Memorial Hospital’s new Female Pelvic Medicine and Reconstructive Surgery division. His specialty, also known as urogynecology, includes gynecology, obstetrics and urology. He treats women for incontinence, prolapse and other conditions.
To treat Kravets’ prolapse, Gruber stitched together the front and back walls of the vagina to shorten the vaginal canal, a procedure known as colpocleisis. He also placed a mid-urethral sling, a small piece of mesh that supports the urethra and prevents urinary leaks during physical activity.
Kravets says her condition has improved dramatically since the November procedure.
“I’ve had not a problem in the world,” she says. “It was very uncomfortable, and that’s all gone. That’s all disappeared.”
Gruber came to Sibley in September 2020, after retiring from the U.S. Air Force as a colonel. He was at Walter Reed National Military Medical Center for 13 years, including five as fellowship director for urogynecology.
At Sibley, Gruber treats women with a variety of pelvic and urological issues. When appropriate, he tries nonsurgical treatments before recommending surgery. “Maybe they’ll end up wanting surgery down the line, but I don’t push it because it’s not right for everybody,” he says.
Nonsurgical treatment options include medication; electrical stimulation therapy for overactive bladder; bladder Botox, which helps the muscles involved in urination relax for patients with incontinence issues; and pessary, a silicone device that sits in the vagina to support areas affected by prolapse.
When performing surgery, Gruber uses vaginal, laparoscopic and robotic methods for a majority of procedures. Using these minimally invasive techniques means patients have less pain, reduced reliance on pain medications, lower infection rates, reduced hospital stay lengths and a shorter recovery times, he says.
“We expect patients to get out of bed and walk immediately after surgery,” Gruber says.
There are cases, however, in which Gruber more strongly recommends surgery — large prolapse, which can cause kidney damage if the patient is not emptying their bladder; and fistulas, which are abnormal connections between two organs.
To determine the best course of treatment, Gruber and his team perform various tests, including cystoscopy, which examines the inside of the bladder; urodynamics studies, which test how well the body holds and releases urine; and pelvic ultrasounds.
Gruber works closely with Sibley pelvic floor physical therapist Lora John, who treats patients with incontinence, and see patients before and after surgery to help them strengthen their pelvic floor. For patients who don’t immediately want or need to have surgery, physical therapy and other medical interventions offer other therapeutic avenues for treating their condition.
For patients referred to physical therapy, John works with Gruber to help patients strengthen their pelvic floor, recognize the brain-pelvic floor connection — the mental processes that aid in urination and bowel movements — and better utilize the muscles that support the bladder and urethra.
“These issues have a huge effect on people’s daily lives,” says John. “So it’s my job to educate them on how these different body parts can work together to achieve their goals of reducing urgency and incontinence.”
John, whose office is in the same building as Gruber’s, meets regularly with the other Johns Hopkins pelvic floor physical therapists to discuss the latest advancements in the field. “What sets us apart from a lot of other hospitals is that we work together as a team,” she says.
For Kravets, Gruber’s friendly attitude and expertise made for a smooth surgery and recovery process.
“I think he’s pretty terrific,” she says. “Unequivocally, I would absolutely recommend patients go ahead and have whatever procedure they need to have. I have utter confidence in him.”