Johns Hopkins is a national leader in minimally invasive gynecologic surgery and surgical safety and quality, as well as a high-volume center for the advanced treatment of gynecological cancers, endometriosis, fibroids and other complex gynecological conditions.
Experts in the Department of Gynecology and Obstetrics have contributed to setting national standards for minimally invasive gynecologic surgery and best practices in surgical safety, says Amanda Fader, vice chair of gynecologic surgery and director of the Center for Rare Gynecologic Cancers. Based on research by Fader; Rebecca Stone, director of the Kelly Gynecologic Oncology Service; and Stephanie Wethington, director of clinical operations for the service, the Johns Hopkins minimally invasive surgery rate for hysterectomies performed for endometrial cancer and for women at risk of developing a gynecologic cancer is among the highest in the nation. Approximately 80% of hysterectomies for malignant or preinvasive disease and more than 90% of hysterectomies for benign disease are performed using minimally invasive techniques, and over half of all hysterectomies are outpatient procedures.
Additionally, the department has implemented innovative, standardized protocols studied and developed at Johns Hopkins to reduce perioperative complications — such as surgical site infection and venous thromboembolic events — promoting Enhanced Recovery After Surgery (ERAS), lower narcotics use for patients and fewer hospital readmissions.
“Our research and clinical advancements have contributed to the establishment of national benchmarks in minimally invasive gynecologic surgery and surgical quality and safety,” Fader says. “While we are laser-focused on taking the very best care of each patient referred to Johns Hopkins and personalizing that treatment, we’re also always thinking about how to innovate surgery on a larger scale, so that even more women will potentially benefit.”
One of the highest-volume surgical centers for patients with gynecologic cancer in the mid-Atlantic region, Johns Hopkins also treats a large number of patients with genetic mutations or conditions that place them at a higher risk for developing cancer, such as BRCA mutations or Lynch syndrome. In such cases, surgeons can perform minimally invasive preventive surgeries and follow patients and their families in registries for monitoring.
Karen Wang, director of the Division of Minimally Invasive Gynecologic Surgery (MIGS) and the fellowship director of MIGS at The Johns Hopkins Hospital, along with three additional fellowship-trained MIGS surgeons, manages complex benign surgical cases.
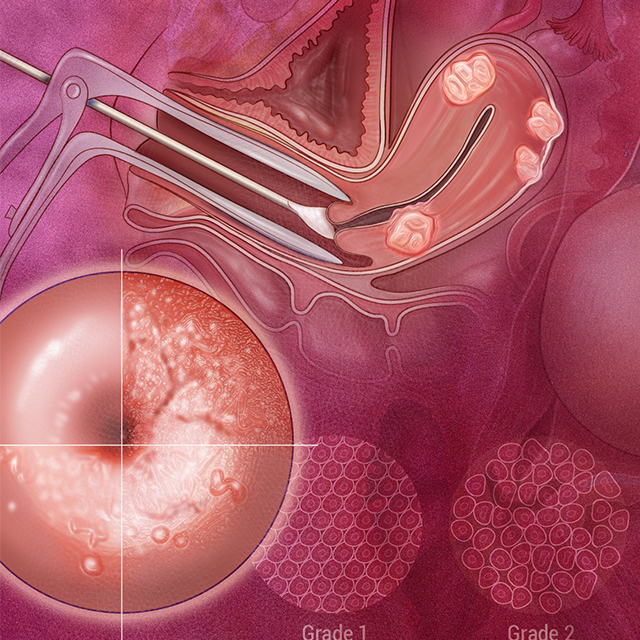
“Due to our high volume, training and experience, physicians will refer cases of higher complexity to us since we have low complication and conversion rates to open surgery,” Wang says. The team commonly manages large uterine fibroids via myomectomy and hysterectomy, advanced stages of endometriosis, large adnexal masses, unusual ectopic pregnancies (cornual and interstitial), and can perform minimally invasive cerclage placement and tubal reanastomosis.
Johns Hopkins’ multidisciplinary, individualized approach to care means the MIGS team collaborates with other specialties, including reproductive infertility, maternal-fetal medicine, colorectal surgery, urology and urogynecology, radiology, and gynecologic oncology for unusual and difficult cases.
Under the leadership of Wang and Kristin Patzkowsky, gynecology director at the Johns Hopkins Health Care & Surgery Center — Green Spring Station, the team has increased the number of in-office procedures it performs at the Green Spring facility, which is home to an ambulatory surgery center. Such procedures include diagnostic and operative hysteroscopy, allowing for quick evaluation and foregoing general anesthesia. The physicians have also led the department in increasing the number of operations — including hysterectomies and other laparoscopic procedures — at the health system’s ambulatory surgery centers by more than 20%. These centers allow surgeons and clinicians to provide care in facilities that are conveniently located close to patients’ homes.