Imagine if after a serious accident, your damaged facial bones could be replaced with tissue made by your own cells. Or if you could pop a pill that could reprogram your immune system to fight a chronic disease, freeing you from a lifetime of medications. While both prospects sound futuristic, scientists and biomedical engineers at Johns Hopkins are working toward these and other advances in tissue engineering.
In the roundup that follows, we highlight just some of the most promising projects now underway — projects that could improve the lives of patients sooner than you might think.
Bone and Facial Reconstruction
Patients experiencing craniofacial bone loss resulting from trauma or cancer removal surgeries have a few options today for reconstructive surgeries. But they all have limitations. Autografts, which take a piece of bone from another body part to transplant to the face, create a second defect. Allografts (which use donor tissue) hold the potential for disease transfer or rejection. Surgeons also can employ materials like metals to serve as an implant; these, too, are subject to possible rejection and don’t move like native tissue.
Enter Warren Grayson. The professor of biomedical engineering has been leading efforts to regenerate bone-like tissue with natural anatomical structure: living tissue that grows and changes with the patient and is constituted from a patient’s own genetic material so it won’t be rejected.
In animal studies, Grayson’s lab has used 3D printers to create scaffolds made from biodegradable polymers combined with other natural materials in the exact shape of the facial defects. Then, researchers take stem cells derived from fat tissue and apply them to the scaffold in a liquid solution. The idea is that the cells will grow throughout the porous scaffold, which provides instructive cues so that they form bone. The scaffold will then degrade away, leaving new, vibrant bone tissue.
Over the years, the Grayson lab has tinkered with various scaffold materials, methods to stimulate stem cells, and recipes for optimal bone growth. The animal studies have demonstrated some bone can be regrown in this manner. “There’s definitely room for improvement,” Grayson says, “but the results have been extremely promising. The data tells you that you can induce the body to go beyond its normal healing capacity.”
In related work, Grayson and colleagues are applying similar processes to regenerate skeletal muscle, and are developing new imaging tools to better study how these materials work once transplanted into the body. Grayson’s group is applying for funding to conduct pilot clinical studies in humans. How quickly things move from there will depend on results and larger-scale clinical trials.

Soft Tissue
People who have lost soft tissues like skin, fat or muscle, whether as the result of a congenital disease or due to trauma or cancer surgery, present a challenge to surgeons. Doctors can transplant tissues like fat harvested from elsewhere in the body, but without supporting blood vessel networks, the transplanted tissue tends to die over time. Some patients don’t have enough soft tissue to spare for the transplant, and synthetic materials such as silicone gels used in breast implants can induce foreign-body reactions by the immune system.
Rather than borrowing tissue, which creates a second defect, plastic surgeon and developmental biologist Sashank Reddy and colleague Justin Sacks (now at Washington University in St. Louis) were looking to develop an off-the-shelf solution. They turned to a collaborator at Johns Hopkins — materials science and engineering professor Hai-Quan Mao — to attack the problem.
“What we aim to do is develop a material that can immediately restore soft tissue defects without invasive surgical procedures, while encouraging the body’s own capacity for repair and regeneration,” Reddy says.
Ideally, says Mao, “the material should be porous enough to allow host tissue to grow into it but also retain its shape and integrity of the repair site, and not lead to scarring and fibrosis by host immune cells. This concept is very easy to understand, but it was difficult to come up with a material design to meet all of those requirements simultaneously.”
The team invented a synthetic soft tissue substitute that is well-tolerated and encourages the growth of soft tissue and blood vessels.
For a model, they observed the microscopic structure of fat, consisting of large cells clustered around an extracellular matrix that provides shape and stability. To devise a new biomaterial, they used a hydrogel made of hyaluronic acid — a naturally occurring component of the body’s extracellular matrix and an ingredient found in more than 90 percent of cosmetic dermal fillers used in this country. Then, they incorporated polyester nanofibers made of the type of material used in resorbable sutures to help the material retain its shape. They broke the fibers into short segments before making the composite gel to ensure easy injection through a needle. The resulting composite gel performed well in preclinical studies, repairing deformities while encouraging growth of new blood vessels.
A company they founded, LifeSprout, is conducting initial clinical trials of small amounts (1 to 3 cubic centimeters) of the soft tissue substitute in the face for softening wrinkles or adding volume to a facial structure.
Additionally, the investigators have been awarded a Maryland Stem Cell Research Fund grant to test this material for larger volume repair, trying to see if they can speed and enhance regeneration by adding fat tissue–derived stem cells.
Peripheral Nerves
A couple of years ago, Johns Hopkins plastic and reconstructive surgeon Sami Tuffaha approached Hai-Quan Mao with a vexing problem.
Tuffaha is an expert on targeted muscle reinnervation, a peripheral nerve repair procedure for amputees during which each severed nerve at the amputation site is sutured to a smaller motor nerve supplying a neighboring muscle. This helps prevent the formation of painful neuromas — disorganized neural growth on the ends of severed nerves. However, the size difference between the two nerves being connected creates additional technical challenges and still leads to partial neuroma development at the repair site, and is thought to lead to treatment failure in some 30 percent of patients.
Three engineering undergraduate students stepped up to find a solution, devising a flexible, cone-shaped device as a conduit to guide regenerating nerve fibers across the repair site, from the larger to the smaller nerve, in an orderly fashion. The biodegradable device is filled with a hydrogel that includes an inhibitory proteoglycan to block a portion of the regenerating nerve fibers and prevent the smaller recipient nerve’s capacity from being overwhelmed. Together, these components guide and regulate nerve regeneration across the size-mismatched repair site and into the target muscle, thereby preventing painful neuroma formation.
The team observed the device achieved a tapered, orderly regeneration of nerve fibers, including pain fibers, within the device. The team has filed a provisional patent on its work under a spin-off company named Innerva and is continuing to refine it. Studies being performed to test the efficacy of the device are being led by medical student Erica Lee, who has established a small animal model for neuropathic pain resulting from neuroma formation.
Beyond neuropathic pain, peripheral nerve injuries also cause debilitating paralysis and numbness, Tuffaha says. Following surgical repair, there are no available drugs to help improve the process of nerve regeneration, and muscles lacking nerve supply undergo progressive, irreversible atrophy while waiting for that regeneration to happen — potentially downgrading the amount of motor function a patient can achieve.
To that end, Tuffaha and Mao developed a delivery system to treat affected nerve and muscle tissue with insulin-like growth factor-1 (IGF-1), which has been known to promote nerve regeneration and limit muscle atrophy. The protein therapeutic is encapsulated in nanoparticles, which are suspended in a specialized gel and injected along the injured nerves and into target muscles lacking nerve supply. There, it slowly releases IGF-1 over a six-week period. Reinjections every six weeks are performed using ultrasound guidance. Studies in small animal models and primates appear promising, with substantial improvement in functional recovery, Tuffaha says.

Cellular-Level Technologies
The human body holds trillions of cells that function like tiny computers, processing inputs that direct them to grow, divide, specialize or self-destruct, explains biomedical engineer Jordan Green, who leads the Biomaterials and Drug Delivery Laboratory.
Green’s lab has taken a cue from viruses, which trick cells into letting them enter and then use this space to replicate, to focus on developing novel, biodegradable nanobiomaterials that can deliver medications or genetic material in miniature packages (1/1,000th the size of a human hair) directly to specific types of cells, thereby reprogramming them from the inside out.
“The wave of the future is doing in situ tissue engineering using administered gene therapy and immunotherapy to promote healing and regeneration of tissues within the body,” Green says. “We’re going to see these technologies more and more.”
The process could be used to deliver DNA and RNA to cells to turn genes on or off individually or in combination. This holds potential for common genetic conditions such as cystic fibrosis or hemophilia as well as more complicated diseases like cancer or diabetes, Green says. It even can help hit targets traditionally seen by pharmaceutical companies as “undruggable.”
Green and colleagues also are working on developing different sizes and shapes of artificial immune cells to mimic biological cells, with proteins added to the surface that teach native immune cells what to do, such as attacking cancers or promoting tissue repair. A recent study demonstrated that nanoparticles the lab developed using molecules called poly(beta-amino esters) (PBAE), along with an engineered sequence of DNA, could reprogram liver cancer cells to secrete a protein called TRAIL that initiates cancer cell death. Combining this approach with small-molecule drugs could offer a new potential approach for cancer treatment.
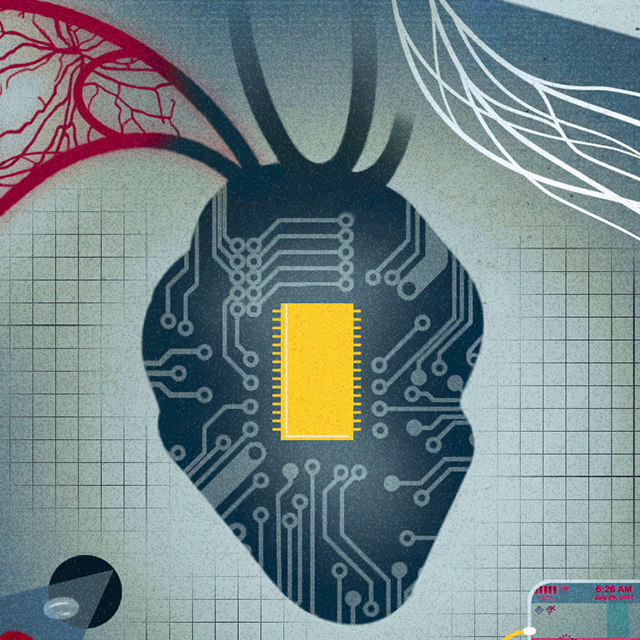
Heart
Deok-Ho Kim’s research in cardiac tissue engineering is out of this world. Kim (Ph.D. ’10), an associate professor of biomedical engineering and medicine, has developed 3D engineered cardiac tissues that mimic the microarchitecture and function of human heart tissue on a microchip.
The work made news headlines in March 2020 when Kim and colleagues sent some of their miniaturized heart tissues in SpaceX to the International Space Station for a month, to study how space travel and weightlessness — which has been known to simulate accelerated aging — affects the heart’s structure and function. Over a month’s time, Kim’s team observed that contractile force and heart function declined compared to similar tissues studied on Earth.
Sponsored by the National Institutes of Health and NASA, the team now is gearing up for a second space launch in fall 2022. This time, the engineered heart tissue chips will be treated with a drug compound or mechanical stimulation, to see if diminishing function can be prevented or lessened. The lab has been testing various interventions using a desktop-sized random positioning machine that simulates microgravity. A companion project funded by NASA is monitoring how radiation from the sun and other elements in space impacts changes in human cardiac tissues.
In other work, Kim, David Kass (a professor of medicine, biomedical engineering and pharmacology) and their colleagues are validating 3D engineered muscular tissues as a “clinical trial on a chip” platform to study cardiac and skeletal muscle deficiencies in human Duchenne and Becker muscular dystrophy, which are inherited conditions marked by progressive muscle weakness. By placing patients’ induced pluripotent stem cell–derived muscular tissues in multiwell plates in the lab, investigators will simulate clinical trials of a novel drug for muscular dystrophy, assessing toxicity profiles, helping determine appropriate doses and potentially personalizing therapy for patients. The trial will study the drug’s performance in a panel of tissues, each with different mutations, as well as some control tissues without mutations.
This type of study could avoid typical problems experienced with early clinical trials such as patient recruitment, patient dropout and potentially harmful side effects. It also may overcome additional concerns, of spending much time and effort performing studies in mice or rats that don’t necessarily translate when the same studies are later performed in humans, Kass says. Creating these miniaturized organoids, be it heart tissue in this case, or tiny models of the kidneys, liver, neurons or brain, is a rapidly exploding area, he says.
“If the hypothesis is right, that this engineered heart tissue derived from human cells will predict what we might find in actual humans,” he says, “then before we go do the clinical trials, we can get data with our engineered heart tissue testing this or other drugs, find out if it works, and hopefully also any side effects we expect.”
Investigators currently are fine-tuning engineering of the heart tissues before testing the drug. However, a platform of other heart and skeletal muscle tissues to test new drugs already is commercially available through Curi Bio, a company Kim co-founded in 2015.
Vasculature
Feilim Mac Gabhann (Ph.D. ’07) likes to ask his students to name the most important organ. The usual suspects emerge: heart, brain, occasionally skin. But it’s a trick question. In Mac Gabhann’s eyes, it’s blood.
“If we didn’t have blood, we’d be a millimeter in size,” says Mac Gabhann, an associate professor of biomedical engineering. “The only reason we can be large, multi-organ organisms is because we have some sort of system that can move oxygen around the body, and communicate among the different organs.”
Most people are familiar with the blood vessels they can see in their arms or their feet, he says. These vessels carry blood to smaller and smaller branches supporting all tissues in the body. Any given piece of tissue is packed with networks of tiny blood vessels, 1,000 times thinner than those we can observe.
Currently, some larger vessels that become injured or diseased, such as in the leg or heart, can be surgically repaired or bolstered, or replaced with synthetic materials. Patches of damaged skin can be repaired through skin grafts. Growing large amounts of tissue, or thicker tissues, however, would be “a major next step,” Mac Gabhann says, and requires creating the right environment to encourage blood vessel growth.
Mac Gabhann’s lab has been using computational modeling — the application of computers to simulate and study complex systems — to study vascular endothelial growth factor (VEGF), a protein family heavily involved in blood vessel growth and development. They want to know why and how these proteins direct the growth of varying blood vessel networks supporting different areas of the body. “If we can understand that,” he says, “we can turn it into a forward engineering problem and design the signals we need to get the kind of networks we want.”
He’s looking primarily at two areas. One is skeletal muscle, trying to figure out some type of medical intervention to help people with peripheral artery disease, a form of blockages of blood vessels in the leg that make it painful to exercise. The other is developmental biology, attempting to understand how blood vessel networks behave in growing tissues.
Pancreas
Joshua Doloff’s lab explores the intersection between therapeutics and living systems, trying to understand what happens when new materials are introduced into the body, and how the host immune system behaves and perceives them. An implanted glucose monitor functioning as an artificial pancreas for a diabetes patient, for example, can be attacked by the body as foreign. This can lead to the development of scar tissue around the device, diminishing its function.
Implanting devices can create a 1–2 punch for the immune system, notes Doloff, who directs the Immunoengineering and Regenerative Medicine Lab at Johns Hopkins. Doctors want to deliver grafts correctly to restore function, but if they’re implanted in the midst of a chaotic autoimmune disorder, it creates two immune challenges: preventing graft rejection and modulating the immune system to prevent further damage. He’s also pursuing immunoengineering studies to help prevent rejection of grafts.
In recent work, Doloff’s team has demonstrated that loading implantable devices with a crystallized immunosuppressant drug that is slowly released at the local area can inhibit the immune response against those devices. The lab also is working on ways to encapsulate islet cells and transplant them into patients with diabetes, potentially to replace nonfunctioning pancreatic cells and eliminate the necessity for insulin injections, or long-term immunosuppressant drugs needed with implanted devices and organ transplants.
“Over the past few years, we’ve gotten a lot of insights into foreign body response,” he says. “We can actually block biomaterial-specific responses quite effectively. And I’m confident that we can do that now for not just biomaterials but even multicomponent devices such as glucose monitors.”
