ALS Research: Discovery and Translation
ALS Research: Discovery
Our greatest limitation to treating Amyotrophic Lateral Sclerosis (ALS) is the lack of understanding what causes or enables sporadic ALS. However, the discovery of human-induced pluripotent stem cells (iPSC) has multiple implications; including helping us understand the disease’s mechanisms.
The ability to create stem cells from skin fibroblasts – cells of connective tissue that produces and secretes fibers e.g. collagen, as well as blood cells – could eliminate the need for using human embryos to derive human embryonic stem cells. This has important ethical implications for the scientific community.
By using adult human cells, we are now able to reprogram these cells to make induced pluripotent stem cells (iPSC) in order to study mechanisms causing ALS. We now have techniques to lead these iPSC down the path to create motor neurons, astrocytes, microglia, oligodendrocytes, Schwann cells and myocytes (muscle cells) from patients with the disease.
Johns Hopkins researchers are uncovering powerful discoveries for this progressive disease. The development of iPSCs from ALS patients with newly identified genes can also provide a powerful tool for investigations into the similarities and differences between different genetic forms of ALS. In addition, iPSCs could also aid in the discovery of candidate drugs for ALS treatment.
We have only begun to scratch the surface in understanding what causes ALS, what factors influence the timing of disease onset, its progression, and its heterogeneity. Our direct involvement with patients in the Johns Hopkins ALS Clinic allows us to answer their questions such as why ALS starts with speech and swallowing problems in some patients, but with limb weakness in others, or, how environmental factors like toxins or traumatic injuries influence the onset of ALS.
The goals of the center will focus on the use of stem cells as tools to foster programs in 'Discovery' and 'Translation'.
How can stem cells speed discovery?
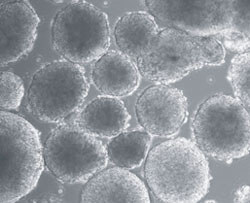 Induced pluripotent stem cells derived from ALS patient
Induced pluripotent stem cells derived from ALS patient- Stem cells made from ALS patients and animal models of ALS can be directed into specific cell subtypes (astrocytes and motor neurons) to study what makes these cells vulnerable. Making stem cells from ALS patients with different kinds of ALS (i.e. those with trouble chewing and swallowing compared to those with arm and leg weakness) could allow us to understand how these cells respond differently.
- Stem cells made from ALS patients with hereditary ALS – the kind that is passed down in families – can be compared to those stem cells from ALS patients with “sporadic” disease – the kind which does not run in families – can help us understand how these forms of ALS differ.
- Stem cells from many ALS patients can be grown in a culture dish to discover what types of environmental factors or toxins influence cell survival.
- Stem cells made from ALS patients and animal models of ALS can be used to screen for drugs that may work to treat ALS (for example, astrocyte stem cells could be used to study drugs that improve the function of astrocytes resulting in neuroprotection. Motor neuron stem cells could be used to study drugs that could keep them from dying or enhance the growth of nerve processes).
ALS Research: Translation
The ALS Center provides flexibility to Johns Hopkins investigators with promising ideas to proceed to the early stages of translation. These early stages of translation can be facilitated through partnerships with the Brain Science Institute (BSI). The ability to take these early discoveries and convert them into potential ALS therapies is illustrated by the fact Johns Hopkins neuromuscular specialists have been heavily involved in clinical trials during the last 25 years. Learn about current ALS clinical trials.
Johns Hopkins has the clinical trials infrastructure and ALS expertise to shepherd promising therapeutics to ALS patients.
