Background
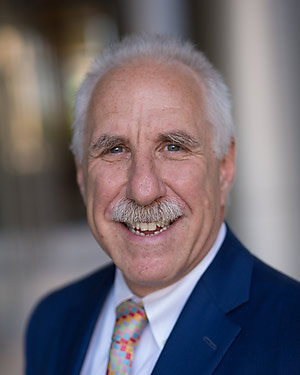
Dr. Paul B. Rothman is a professor of medicine at the Johns Hopkins University School of Medicine. He holds a secondary appointment in the Department of Molecular Biology and Genetics.
A rheumatologist and molecular immunologist, Dr. Rothman serves as the Frances Watt Baker, M.D., and Lenox D. Baker Jr., M.D., Dean of the Medical Faculty. Dr. Rothman served as vice president for medicine at Johns Hopkins University and chief executive officer of Johns Hopkins Medicine from 2012-2022.
Dr. Rothman earned his medical degree (Alpha Omega Alpha) at Yale University School of Medicine. He completed both an internal medicine residency and a rheumatology fellowship at New York-Presbyterian/Columbia University Irving Medical Center, as well as a postdoctoral biochemistry fellowship at Columbia University College of Physicians and Surgeons.
He also holds a Bachelor of Science in biology (Phi Beta Kappa) from the Massachusetts Institute of Technology.
Dr. Rothman’s research focuses on the role of cytokines in the development of blood cells called leukocytes—the abnormal development of which can lead to leukemia—and in immune responses to asthma and allergies.
Before joining the Johns Hopkins faculty in 2011, Dr. Rothman served as dean of the University of Iowa Carver College of Medicine and leader of the university’s clinical practice plan. Prior to that, he served as professor and head of Iowa’s Department of Internal Medicine, with secondary appointments in the Department of Microbiology and the Department of Physiology and Biophysics.
On the faculty of the Columbia University College of Physicians and Surgeons from 1986 to 2004, Dr. Rothman was the founding chief of its Division of Pulmonary, Allergy and Critical Care Medicine. He later served as vice chair for research of the Department of Medicine.
Dr. Rothman’s awards include a James S. McDonnell Foundation Career Development Award, a Pfizer Scholars Award, a Pew Scholars Award, a Leukemia Society of America Scholar Award and the Pharmacia Allergy Research Foundation International Award.
He is an elected member of the American Association for the Advancement of Science, American College of Physicians, Council of the Association of American Physicians and American Society of Clinical Investigation.
Dr. Rothman is a member of the Merck board of directors and receives compensation in the form of income and stock. Dr. Rothman also is a member of the board of directors of the King Faisal Specialty Hospital, for which he receives compensation in the form of income. To submit concerns related to this arrangement, please contact: [email protected].
Dr. Rothman has served as a member of the National Institutes of Health Immunologic Sciences Study Section, the Israel Cancer Research Fund International Scientific Advisory Board, the American Academy of Allergy, Asthma and Immunology Grant Review Committee and the American Thoracic Society Asthma Immunology and Inflammation Program Committee.

Patient Ratings & Comments
The Patient Rating score is an average of all responses to physician related questions on the national CG-CAHPS Medical Practice patient experience survey through Press Ganey. Responses are measured on a scale of 1 to 5, with 5 being the best score. Comments are also gathered from our CG-CAHPS Medical Practice Survey through Press Ganey and displayed in their entirety. Patients are de-identified for confidentiality and patient privacy.