-
D. Brian Foster, Ph.D., M.Sc.

- Director, Laboratory of Cardiovascular Biochemistry
- Assistant Professor of Medicine
-
Nisha Aggarwal Gilotra, M.D.
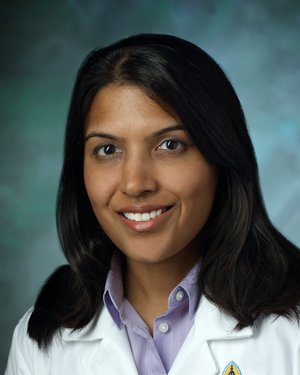
- Director, Cardiac Sarcoidosis Program
- Director, Heart Failure Bridge Clinic
- Medical Director, Heart Failure Disease Management
- Associate Professor of Medicine
Primary Location: Johns Hopkins Outpatient Center (now called Levi Watkins, Jr., M.D., Outpatient Center), Baltimore, MD
-
Steven Hsu, M.D.
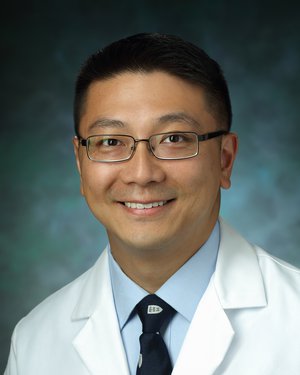
- Medical Director, Mechanical Circulatory Support
- Assistant Professor of Medicine
Primary Location: Johns Hopkins Medicine Cardiology, Bethesda, MD
-
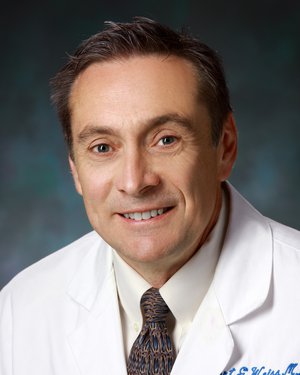
Peter VanDoren Johnston, M.D.

- Medical Director, Cardiac Catheterization Laboratory, Johns Hopkins Howard County Medical Center
- Assistant Professor of Medicine
Primary Location: The Johns Hopkins Hospital (Main Entrance), Baltimore, MD
-
David A. Kass, M.D.

- Abraham and Virginia Weiss Professor of Cardiology
- Professor of Medicine
- Professor of Biomedical Engineering
- Professor of Pharmacology and Molecular Sciences
Primary Location: The Johns Hopkins Hospital (Main Entrance), Baltimore, MD
-
Chulan Kwon, Ph.D., M.S.

- Director, Cardiovascular Stem Cell Program
- Associate Professor of Medicine
- Associate Professor of Biomedical Engineering
- Associate Professor of Cell Biology
-
Brian O'Rourke, Ph.D.

- Robert L. Levy Professor in Cardiology
- Vice Chair of Basic and Translational Research, Department of Medicine
- Director, Bernard Laboratory of Fundamental Research in Preventive Cardiology
- Professor of Medicine
- Professor of Biomedical Engineering
-
Kavita Sharma, M.D.

- Director, Heart Failure & Cardiac Transplantation
- Director, JHU Heart Failure with Preserved Ejection Fraction Program
- Associate Professor of Medicine
Primary Location: Johns Hopkins Outpatient Center (now called Levi Watkins, Jr., M.D., Outpatient Center), Baltimore, MD
-
Emmanouil Tampakakis, M.D.

- Assistant Professor of Medicine
- Assistant Professor of Biomedical Engineering
- Assistant Professor of Genetic Medicine
Primary Location: Johns Hopkins Outpatient Center (now called Levi Watkins, Jr., M.D., Outpatient Center), Baltimore, MD
-
Robert George Weiss, M.D.
- Clarence Doodeman Professor of Cardiology
- Professor of Medicine
- Joint Appointment in Radiology and Radiological Science
Primary Location: The Johns Hopkins Hospital (Main Entrance), Baltimore, MD
Myocardial Biology and Heart Failure
Heart failure means that that the heart is not pumping as it should. It doesn’t mean the heart stops, but rather, that over time it loses pumping function, causing fatigue and shortness of breath. It’s something nearly 5 million Americans face. Understanding the cellular basis of heart failure before and after it happens, along with genetic mutations and differences in men and women, helps researchers target research and create clinical trials. The innovative new methods researched ultimately impact patient care.
Understanding the Cellular Basis of Heart Failure
For instance, it may sound counterintuitive, but researchers at Johns Hopkins say that disrupting the electrical activation of the heart for a few hours a day may be exactly what it needs to avoid heart failure — it actually makes the heart stronger. Similarly, understanding the cellular basis of heart attack and heart failure by researching how modifying calcium, nitric oxide, reactive oxygen species, intermediate filaments and proteins such as CamKII, PDE-9 and PKG can forge new ways to treat the failing heart. Besides leading to drug therapies, these advances are leading to biological treatments, where targeting antibodies or specific genes can be introduced to alter heart muscle behavior in ways that counter the underlying disease.
Genetics, Sex and Heart Failure
Fruit flies aren’t the first thing to come to mind when thinking of muscles, but researchers are using them to study the heart. Drosophila melanogaster, the fruit fly, expresses heart and skeletal muscle much like that found in humans — in fact, made up of much the same protein building blocks. Humans with mutations in a single molecule in a muscle protein can develop severe heart disease. Researchers are using the fly heart to study how this happens and then testing drugs that might fix it.
Our clinical researchers are learning about the abnormal right heart in diseases where pressures in blood vessels of the lung increase greatly. Women and men are different in many ways, and heart failure is one of them. We are studying heart failure in women, notably after menopause, to discern how the hormone changes impact pathways that contribute to this disease and specific ways this could be targeted by therapies.
Regenerative Therapies
Many new methods are being researched once a patient has already had heart failure or a heart attack. We are identifying new protein pathways that are abnormally active in the diseased heart and finding new ways to counter them. Stem cell and regenerative therapies for heart failure and heart attack include using cells derived from human blood or skin that are changed to a heart stem cell. Laboratories are developing methods to implant these stem cells into the heart, including implantable bioreactors to keep them active and tissues printed by a biological 3-D printer.
#TomorrowsDiscoveries: Heart Attack in a Dish
Dr. Brian O’Rourke and his laboratory study how mitochondria, the cellular powerhouses of the heart, contribute to heart attacks and heart failure.
Related Articles & Press Releases
- Unsynching the Heartbeat a Bit Each Day Halts Worsening Heart Failure
- Johns Hopkins Researchers Identify 'Missing Culprit' in Heart Failure
- How Oxidizing a Heart ‘Brake’ Causes Heart Damage
- Viagra's Other Talents, To Help a "Signaling" Protein Shield the Heart from High Blood Pressure Damage
- Johns Hopkins Researchers Show How a Modified Pacemaker Strengthens Failing Hearts
- Flies Help Researchers Get to the Roots of Human Disease
- Getting to the Heart of Fruit Fly Research
- Fruit Fly Muscles with a Hypertrophic Cardiomyopathy Mutation Don’t Relax Properly
- Researchers Reverse Heart Failure in Marfan Mice
- Gender Differences Stand Out in Measuring Impact of Viagra as Therapy for Heart Failure
- Rare Type of Immune Cell Responsible for Progression of Heart Inflammation to Heart Failure in Mice
- Mouse Studies Shed Light on How Protein Controls Heart Failure
- Fruit Fly Muscles with a Hypertrophic Cardiomyopathy Mutation Don’t Relax Properly
- Severe Obesity Revealed as a Stand-Alone High-Risk Factor for Heart Failure
- Sex Hormone Levels Alter Heart Disease Risk in Older Women
- Six Years of Exercise -- or Lack of It -- May Be Enough to Change Heart Failure Risk
- Heart Failure: The Alzheimer’s Disease of The Heart?