Adrenalectomy
An adrenalectomy is a surgical procedure to remove the adrenal gland if it is cancerous and/or producing too much hormone. The adrenalectomy is typically performed through small incisions (minimally invasive) although it also may be performed as an open surgery.
Adrenal Gland Removal
There are several methods for surgical removal of an adrenal gland. You and your surgeon will discuss which type of surgery is best for you.
Laparoscopic Adrenalectomy
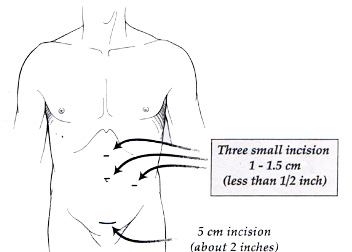
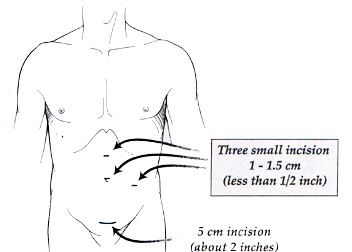
A laparoscopic adrenalectomy is a minimally invasive procedure that uses small incisions and tools to access the adrenal gland. The surgery is performed through three to four small (0.5–1 centimeter incisions made in the abdomen. A telescope and small instruments are inserted into the abdomen through these small incisions, which allow the surgeon to completely remove the diseased adrenal gland. The adrenal gland is placed in a plastic sack and removed intact through one of the incisions.
Laparoscopic adrenalectomy is performed under general anesthesia and usually is completed in one to two hours.
With this less invasive approach to adrenalectomy, patients report less pain after surgery and faster recovery times. When compared to conventional open surgery adrenalectomy, laparoscopic adrenalectomy has resulted in significantly less pain after surgery, a shorter hospital stays, earlier return to work and daily activities, more favorable cosmetic results and outcomes identical to those of open surgery for noncancerous (benign) tumors.
Recovery from Laparoscopic Adrenalectomy
Most patients recover from laparoscopic adrenalectomy quickly. They often stay overnight in the hospital, then recover at home for one to three weeks until returning to full function.
Johns Hopkins Comprehensive Adrenal Center

Johns Hopkins adrenal surgeons are high-volume surgeons and experts in complex and routine adrenal gland conditions, second opinion imaging and pathology review in case discussion with experts in the field. Patients referred to Johns Hopkins for an adrenalectomy receive multidisciplinary care through the Johns Hopkins Comprehensive Adrenal Center.
Posterior Retroperitoneoscopic Adrenalectomy (PRA)
This type of minimally invasive adrenalectomy is performed through the back rather than through the abdomen. Since the adrenal gland and kidney are in the back part of the abdomen — called the retroperitoneum — this approach is direct and does not encounter the other organs in the abdomen. The surgery, associated pain and recovery are similar to those for laparoscopic adrenalectomy.
Robotic Adrenalectomy
Robotic-assisted adrenalectomy, commonly referred to as robotic adrenalectomy, is a type of minimally invasive surgery during which the surgeon controls small instruments hooked onto robotic arms.
Robotic surgery’s approach, recovery and results are similar to those of minimally invasive laparoscopic adrenalectomy.
Open Adrenalectomy
An open adrenalectomy is surgery using an incision in the abdomen. Most adrenal cancers require this form of surgery, which requires a larger incision, because they must be completely removed in one piece to prevent spreading the disease throughout the abdomen.
Recovery from Open Adrenalectomy
Patients having open adrenalectomy require a hospital stay of about four or five days and then need about four to six weeks to recover at home.
Partial (Cortical-Sparing) Adrenalectomy
Certain types of adrenal tumors can be removed safely without removing the entire adrenal gland. This approach may be recommended for patients with tumors on both adrenal glands, like pheochromocytomas.
Bilateral Adrenalectomy
Some people need to have both adrenal glands removed. This is rare and may be a treatment for Cushing’s disease. If both adrenal glands are removed, the patient must take steroid hormones (typically hydrocortisone and fludrocortisone) twice daily. In these cases, although living without adrenal glands requires lifelong medications, many people feel better after adrenalectomy. Usually this surgery can be performed laparoscopically.
Reasons for an Adrenalectomy
You may need an adenectomy if you have been diagnosed with:
- A functional adrenal tumor: a functional adrenal tumor causes an imbalance of adrenal hormones. Removal of the tumor may restore normal adrenal function.
- Large adrenal tumor: Other reasons to remove an adrenal gland are for adrenal tumors that are greater than 4 to 6 cm or have grown in size. In general, biopsy of the adrenal gland is not recommended before removal, even in cases of suspected cancers. The two main types of cancer in the adrenal gland are primary adrenal tumors (adrenocortical carcinoma) and metastasis to the adrenal gland (spread from tumors from another organ).
- Metastasis to the adrenal gland: Cancer that started at another site can spread to the adrenal gland. The most common types of cancer that spread to the adrenal gland are melanoma, breast cancer, lung cancer, kidney cancer and colorectal cancer. These types of cancers can often be removed from the adrenal gland with minimally invasive surgery if needed. The decision whether to perform surgery depends on the state of the primary cancer.
Adrenocortical carcinoma: This rare, cancerous tumor of the adrenal gland can grow quickly and may be associated with abnormal hormone production. If this type of tumor is suspected, it should not be biopsied. In most cases, if the tumor can be removed with surgery, it is performed through an open incision.