Hip Replacement Surgery
What You Need to Know
- Hip replacement can address hip pain and stiffness for people with arthritis, avascular necrosis or other forms of hip joint damage.
- During a hip replacement surgery, an orthopaedic surgeon replaces both ends or one end of the damaged hip joint with artificial parts.
- There are various surgical approaches to hip replacement surgery, including minimally invasive options that may be appropriate for some patients.
- Recovery and rehabilitation help you restore mobility and return to activities with less pain.
What is a hip replacement?
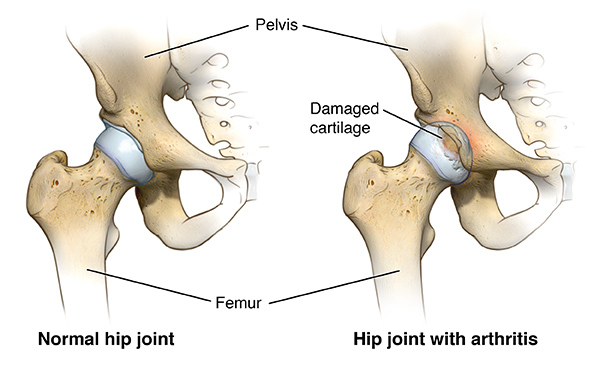
Hip replacement, also called hip arthroplasty, is a surgical procedure to address hip pain. The surgery replaces parts of the hip joint with artificial implants. The hip joint consists of a ball (at the top of the femur, also known as the thigh bone) and a socket (in the pelvis, also known as the hip bone). Hip replacement surgery includes replacement of one or both parts. The goal of the procedure is to allow you to resume daily activities and exercise with less pain.
Who can benefit from a hip replacement?
Your doctor may recommend hip replacement if you have significant pain, inflammation and damage to your hip joint due to conditions such as:
- Osteoarthritis (most common)
- Rheumatoid arthritis
- Osteonecrosis (avascular necrosis)
- Injury such as hip fracture
- Tumor in the hip joint
How do you know if you need a hip replacement?
When your quality of life suffers due to hip pain, it may be time for hip replacement. Signs of declining quality of life include:
- Inability to get restful sleep because of pain
- Difficulty doing simple tasks such as getting dressed or climbing stairs
- Inability to fully participate in the activities you enjoy
At first, your doctor may recommend other treatments such as medicine for pain or inflammation, walking aids, joint injections and physical therapy. If these measures do not relieve pain and stiffness, hip replacement surgery may be necessary to restore function and improve quality of life.
Types of Hip Replacement Surgery
Several factors help determine the type of hip replacement you may need. Your doctor will consider each of the following when planning your care.
Total and Partial Hip Replacement: Which parts need to be replaced?
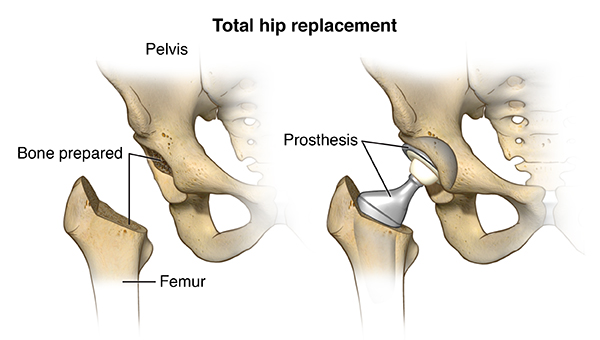
During total hip replacement (total hip arthroplasty), both the ball and the socket are replaced. A partial hip replacement only replaces the ball (the head of the femur).
Anterior, Posterior and Lateral Hip Replacement: How will the surgeon access the hip?
An orthopaedic surgeon can access the hip from different angles. Three common ways to access the hip joint are:
- From the front (anterior approach to hip replacement)
- From the side (lateral approach to hip replacement)
- From the back (posterior approach to hip replacement)
Approaches to Hip Replacement Surgery | Dr. Savya Thakkar
Traditional and Minimally Invasive Hip Replacement: How large will the incision be?
Minimally Invasive Hip Replacement
Minimally invasive hip replacement aims to minimize the impact of surgery on healthy tissues, such as muscles and blood vessels. While anterior hip replacement has been marketed as a minimally invasive approach, orthopaedic surgeons nowadays use minimally invasive techniques with all surgical approaches to access the hip. Your surgeon will discuss which approach might offer the best result.
When the surgery is minimally invasive, the surgeon accesses the hip joint though one or two small incisions by moving the muscles aside. This approach may have advantages, such as:
- Lower risk of muscle damage
- Less pain
- Quicker and easier recovery
- Less limping
- Shorter hospital stay
- Lower chance of hip dislocation
Minimally invasive hip replacement is not appropriate for all patients. Your age, weight, fitness level and other factors will help the surgeon decide if you are a good candidate.
Traditional Hip Replacement
A traditional hip replacement includes a single, large incision that helps the surgeon gain access to the hip, usually through the side (lateral approach) or from the back (posterior approach).
Recovery from a traditional hip replacement can take time, because the surgeon needs to cut through or detach some muscles and tendons to get to the joint. (The muscles and tendons are repaired when the hip implants are in place.) You may be at risk for a dislocation until all of your new hip’s supportive structures are healed.
Talk with your orthopaedic hip surgeon to discuss which surgical approach may be best for you.
Discussing the Best Approach With Your Doctor
The surgical approach your doctor will recommend depends on several factors, including how the surgeon will gain access to the hip, the type and style of the implant and how it will be attached, and your age and activity level, and the shape and health of the hip bones. The likelihood of future surgery also figures into the decision, because some surgical approaches and types of implant attachment can make a revision surgery easier or more challenging.
As part of the evaluation for surgery, your orthopaedic surgeon will discuss the options of minimally invasive surgery or traditional hip replacement, as well as how he plans to perform the surgery and what type of implant will be used.
Hip and Knee Replacement at Johns Hopkins
Parts of a Hip Replacement Implant (Hip Prosthesis)
The hip replacement implant, also called hip prosthesis, has two parts:
- A ceramic ball attached to a metal stem, which is inserted into the thigh bone (femur) for stability
- A metal cup (typically made of titanium) with an inner plastic layer, which is attached to the socket part of the hip joint (acetabulum) to allow the prosthetic joint to rotate smoothly
In the past, the ball was made of metal as well, but the current standard is ceramic.
Types of Socket Implant Attachment
- Uncemented prosthesis attaches with a porous surface, which allows bone to grow over time and hold it in place.
- Cemented prosthesis attaches with bone cement.
Both uncemented and cemented approaches can work well to secure the implant. As hip replacement techniques have evolved over the years, the cement used has improved, as have methods to encourage natural bone re-growth.
For some hip replacements, the surgeon will combine methods. He or she might prefer to use cement on the femoral stem while using an uncemented attachment on the socket piece that fits into the hip bone.
Can you get both hips replaced at the same time?
Both left and right hips can be replaced during a single surgery. A double hip replacement is also called a bilateral hip replacement. If you are having issues with both hips, your doctor might recommend a double hip replacement if you are in good health and can tolerate a longer surgery and a more challenging recovery.
What happens during a hip replacement surgery?
Hip replacements are performed in a hospital or surgery center. They are often considered outpatient procedures, even though you might need to stay a night or two for observation or to resolve complications.
A typical, uncomplicated total hip replacement surgery has the following steps.
- Once in the operating room, you will get an intravenous (IV) line in your hand or arm. A urinary catheter may be inserted as well.
- You will receive anesthesia, either general (whole body) or below-the-waist (epidural), depending on the recommendation of your anesthesiologist and orthopaedic surgeon.
- The surgeon will place you in an appropriate position to access the hip joint and make an incision. The incision’s location depends on which approach (front, back or side) the surgeon uses.
- The surgeon will remove the head of the femur (the ball part of the joint) and make an opening in the top of the femur. He or she will then insert the stem of the ball prosthesis, with or without cement. The ceramic replacement head will then be attached to the top of the femur implant.
- The surgeon will then remove the damaged cartilage from the acetabulum (the socket part of the joint) and attach the new cup.
- Your surgeon will bend and move your leg to ensure that it functions properly.
- Layers of tissue will be closed with stitches that dissolve. The outermost layer of skin is closed with surgical glue. No stitches will need to be removed after your surgery.
- You will be taken to the recovery room for a couple hours and then transferred to a hospital room. The surgeon will let you know when it is safe to go home, which could be the same day, depending on your condition.
How long does a hip replacement surgery take?
On average, hip replacement surgeries last about two hours. A partial hip replacement might require less time, and a double hip replacement may take longer. Complications during surgery might also extend the surgery time.
You may need imaging, such as an X-ray, immediately after the procedure and during recovery, to confirm that your surgery was successful and that your new hip is healing well.
After a Hip Replacement
Hip replacement recovery starts right away. You will be encouraged to get up and move around as soon as possible after surgery. Patients who don’t have other health conditions can go home as soon as they demonstrate that they can walk, climb stairs, and get in and out of a car.
Some patients might spend time in an inpatient rehabilitation unit to prepare for independent living at home. Whether you go home or to a rehabilitation unit after surgery, you will need physical therapy for several weeks until you regain muscle strength and good range of motion.
The surgeon, physical therapist or occupational therapist can advise you on when you are ready to walk with or without assistance, and how to manage your pain. The provider will discuss your rehabilitation needs, what to expect in the days and weeks ahead, and how to make the most of your recovery. Your motivation and cooperation in completing the physical therapy is critical for an effective recovery process and overall success of the surgery.
While you recover, be sure to:
- Keep the surgical area clean and dry. Your doctor will give you specific bathing instructions.
- Take all medications as directed.
- Keep all the follow-up appointments with your surgeon.
- Attend physical therapy and complete home exercises.
- Resume your normal diet unless otherwise instructed.
- Elevate the leg and use ice to control swelling.
- Do not drive until your doctor says it is safe to do so.
Some fluid might drain from your incision. This is normal during the first few days after surgery. Let your surgeon’s office know right away if you have increased redness, swelling or draining from the incision, high fever, chills or severe pain. Also contact the office if your pain is not improving.
What are the risks of hip replacement surgery?
Most patients do well with hip replacement. As with any surgical procedure, there are some risks during and after a hip replacement:
- Bleeding
- Infection
- Blood clots in the legs or lungs
- Leg length discrepancy
- Injury to nearby nerves
- Fracture
- Continued pain or stiffness
- Dislocation
- Loosening or wearing out of the prosthesis
- Unrelieved joint pain (this may be temporary)
In very, very rare cases of bone surgery, particularly procedures using cement, an embolism (blockage) can occur if fat from the bone marrow enters the bloodstream. A fat embolism can raise the risk of a heart attack or stroke.
There may be other risks depending on your medical condition. Be sure to discuss any concerns with your doctor before the procedure and ask which risks are highest for you.
After the surgery, notify your doctor if you notice any of the following:
- Fever
- Redness, swelling, or bleeding or other drainage from the incision site that doesn’t stop after a few days
- Increased pain around the incision site
- Pain in the lower leg that is unrelated to the incision
- New or increased swelling of the lower leg
Call 911 or go to an emergency room if you experience:
- Chest pain
- Shortness of breath
Revision Hip Replacement Surgery
Your hip implant may wear out or loosen over time. It might also become damaged if you have an injury or dislocation. You may need a revision surgery to replace the damaged parts of the prosthesis. Most hip prostheses last 20 years or longer. You might be able to extend the life of your implant by doing regular low impact exercise, avoiding high impact exercise (such as jogging) and taking precautions to avoid falls.
A rare risk of hip replacement is infection, which can happen if bacteria circulating in the bloodstream get caught in the prosthetic pieces. An infection may require a revision surgery to remove the infected tissues, and a course of antibiotics to kill the bacteria. When the infection is gone, a new prosthetic can be put back in.
If you had a partial hip replacement (only the ball part of the joint), you may need a revision down the road to replace the socket as well.







