Inclusion Body Myositis
Inclusion body myositis (IBM) causes muscle weakness that may worsen over time and damage the muscles. The rate of this decline varies among individuals. This degenerative muscle condition is more common in older adults, especially men over 50.
What You Need to Know
- Inclusion body myositis is a rare condition that causes muscle weakness and damage.
- Symptoms of IBM vary, but usually include progressive weakness in muscles of the hand, forearm, thigh and lower leg.
- Diagnosing IBM can be challenging because the symptoms are not unique to this condition. Muscle biopsy is often needed to narrow down the diagnosis.
- There is no effective treatment for IBM, but a combination of medication and rehabilitation therapy can be beneficial for many patients. There are also ongoing clinical trials in IBM with a goal to find an effective therapy.
What is inclusion body myositis?
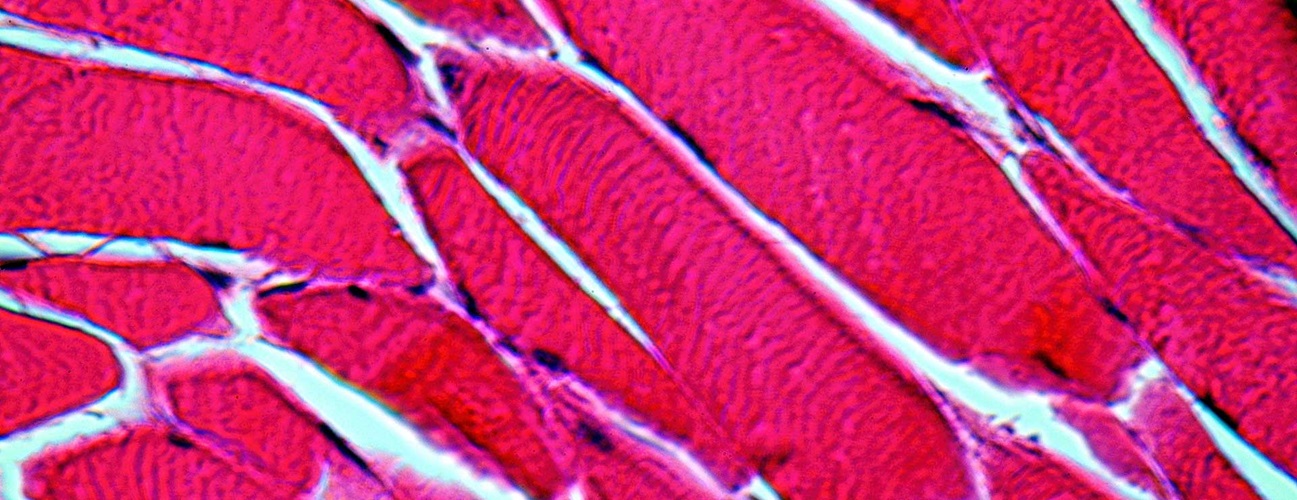
Myositis is a broad term that describes muscle inflammation. Inclusion bodies are abnormal structures found in muscle cells that can be seen in muscle biopsies of patients with IBM. The presence of inclusion bodies sets apart this type of myositis from similar conditions such as polymyositis.
Symptoms of Inclusion Body Myositis
Inclusion body myositis causes muscle weakness and degeneration in certain areas of the body. The areas affected the most are usually wrists and fingers, front of the thighs and front of the legs below the knee.
As the muscles in these areas gradually waste away, you may experience the following symptoms:
-
Frequent tripping and falls
-
Muscle weakness in the quadriceps, hand, forearm and ankle
-
Knees giving way
-
Loss of ability to walk or dexterity in your hands
-
Difficulty raising the front of your foot (drop foot)
These symptoms usually develop gradually — over a period of months and, sometimes, years. Symptoms are not always present or equally felt on both sides of the body. The location, severity and onset of symptoms may vary from person to person.
How is inclusion body myositis diagnosed?
As you get older, you may experience many health issues. Muscle weakness is often expected with age and is easy to dismiss. Because myositis is rare, many cases of IBM go undiagnosed or misdiagnosed for years after the first symptoms appear. Not many doctors have seen patients with myositis, and even fewer have treated them. It is best to seek an opinion of a myositis specialist if you or your doctor suspect you may have this disease.
To diagnose inclusion body myositis, a specialist may use all or a combination of these methods:
-
Physical examination and medical history
-
Blood tests to look for disease-specific enzymes or antibodies
-
Nerve conduction studies to measure any interruptions in the nerve signal
-
Electromyography to help rule out neurological conditions
-
Muscle biopsy to verify the presence of inclusion bodies to confirm the diagnosis
-
Genetic testing
Causes of Inclusion Body Myositis
Inclusion bodies are found in two distinct, yet related, conditions. Although their symptoms and diagnosis may be similar, their origins differ:
-
Sporadic inclusion body myositis (s-IBM) has no known causes. It has an autoimmune component, which means the body attacks itself. However, other factors could be at play, and it’s still unknown what triggers s-IBM.
-
Hereditary inclusion body myopathy (h-IBM) can be linked to genetic factors. It is called “myopathy” rather than “myositis” because muscle inflammation is generally not involved. It usually manifests itself much earlier than s-IBM — sometimes as early as the 20s. This disease also tends to spare the thigh muscles until the advanced stages.
Inclusion Body Myositis Treatment
There is currently no treatment that can reverse or rid your body of inclusion body myositis. Despite the autoimmune component, IBM doesn’t respond well to immunotherapy. However, it could be beneficial to some patients, especially those with other autoimmune disorders.
Many inclusion body myositis patients could also benefit from physical, occupational and speech therapy.
-
Physical therapy can help maintain strength and mobility as long as possible.
-
Occupational therapy can help make daily activities easier and help avoid falling injuries.
-
Speech-language therapy can help manage swallowing problems.
Because inclusion body myositis damages the muscles, exercising should be done under the guidance of a specialist. A rehabilitation physician or a neurologist specializing in myositis can help you develop a custom exercise plan.
There are also ongoing clinical trials for myositis. Ask your doctor for more information.
Due to the chronic nature of IBM, some patients may also benefit from consulting a rehabilitation psychologist to manage psychological aspects of living with myositis.
Prognosis and Complications of Inclusion Body Myositis
Although there is no effective treatment, having inclusion body myositis does not directly affect your life expectancy. However, it may shorten your life span indirectly through the dangerous consequences of losing your muscle strength. As the muscle weakness gets worse and spreads, you may experience:
-
Swallowing difficulties (dysphagia) that may lead to choking
-
Disrupted breathing from the weakened diaphragm
-
Injuries from falls
-
Poor mobility that may require use of assistive devices, such as a wheelchair
-
Pressure sores, muscle atrophy and other consequences of poor mobility
A myositis specialist can help you manage these and other aspects and risks of living with inclusion body myositis.