The mission of the Johns Hopkins University Division of Geriatric Medicine and Gerontology is to provide the highest level of health care to older adults, and to discover, translate and teach new knowledge through education and research. We aim to be an inclusive and vibrant academic community that sets the international standard for clinical care, education, and scientific discovery focused on improving the health of older adults.
-
Clinical Services
We offer long-term and community care through a number of clinical services, including the Beacham Center’s primary care services, inpatient consultative services, individualized care program (ElderPlus PACE), and home-based medicine.
-
Research
Whether exploring the biology of healthy aging, studying the health services offered to adults or looking at a multi-disciplinary approach that combines policy and medicine, the Division’s researchers are pushing the level of knowledge and quality of service further.
-
Education & Training
The Division’s education and training programs offer mentoring and individualized instruction. Programs include summer training, clinical and research fellowships and continuing education programs to prepare the next generation to better serve an aging society.
News and Announcements
-
New Research Regarding Cancer Screening for Older Adults
Justine Enns, an MSTAR student, led an important study regarding primary care doctors’ approaches and priorities for cancer screenings among older adults.

-
Dr. Roland Thorpe, Jr. Appointed Associate Vice Provost of Faculty Diversity
Dr. Roland Thorpe Jr., has been appointed as the inaugural Associate Vice Provost of Faculty Diversity at Johns Hopkins. Learn more about his plans and initiatives.

-
Caregiving Strain Among School of Medicine Faculty
Doctors at Johns Hopkins research about medical faculty who are also caregivers. Researchers found higher rates than the national average, 90% of whom reported caregiving strain among medical faculty aged 55 or older across 14 US schools.

Division History
Created in 1983, the Johns Hopkins Division of Geriatric Medicine and Gerontology grew out of the Division of Chronic and Community Medicine begun in 1963 on the campus of Baltimore City Hospitals (which is now the Johns Hopkins Bayview Medical Center). At that time, Mason F. Lord, MD, instituted a community outreach program and formal review for each patient in the existing nursing home and chronic hospital on the site with the goal of finding placements for the patients at community sites whenever possible.
His pioneering work on behalf of the institutionalized elderly continues to inspire the division as it evolves. While all of our directors have used Dr. Lord’s philosophy to guide their efforts, two other directors stand out for their contributions.
-
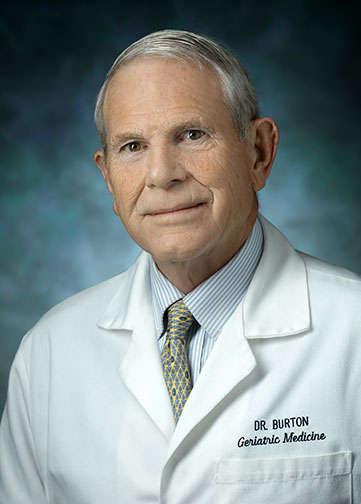 In 1998, John R. Burton, MD, became the division’s director, having served as clinical director previously. Through his vision, the division continued to expand and grow its clinical, educational, and research programs.
In 1998, John R. Burton, MD, became the division’s director, having served as clinical director previously. Through his vision, the division continued to expand and grow its clinical, educational, and research programs.Major clinical programs begun or developed under Dr. Burton's leadership include: Elder House Call Program, Hospital at Home, Program for All-inclusive Care of the Elderly (PACE), and the Orthopedic-Geriatric Medicine Hip Fracture Service. The Division honored his work by renaming the Johns Hopkins Care Center, built in 1991, as the John R. Burton Pavilion.
-
 Under the leadership of Linda Fried, MD, MPH, who became director in 2002, the division's research programs took a major leap forward. She had already created the Center on Aging and Health (COAH), a multi-disciplinary research group focusing on clinical and population-based research, on the Johns Hopkins Hospital campus in 1998. As director, she expanded COAH’s multi-disciplinary research through a new Claude D. Pepper Older Americans Independence Center; added a Center on Aging and Health on the Bayview campus, focused on health services and research or multi-morbidity; and created the Biology of Frailty program.
Under the leadership of Linda Fried, MD, MPH, who became director in 2002, the division's research programs took a major leap forward. She had already created the Center on Aging and Health (COAH), a multi-disciplinary research group focusing on clinical and population-based research, on the Johns Hopkins Hospital campus in 1998. As director, she expanded COAH’s multi-disciplinary research through a new Claude D. Pepper Older Americans Independence Center; added a Center on Aging and Health on the Bayview campus, focused on health services and research or multi-morbidity; and created the Biology of Frailty program.Today, thanks to these exemplary leaders and others like them, the Division's research now spans a broad spectrum from the biology of aging to health policy, with a focus on facilitating the translation of research discoveries into applications that will directly improve the health of older adults.
Notable accomplishments of the Mosaic Initiative
-
An annual event that serves to discuss and educate on a number of topic relating to diversity and inclusion within healthcare. Previous topics have included training and career transitions for under-representative minorities and members of the LGBTQ community.
-
These are created messages that are disseminated in the workplace to promote civility and respect between our fellows, faculty and staff.
-
The Mosaic Initiative has collaborated with other medical schools to improve training and career pathway guidance. Previous collaborations include those with Howard University.
Former fellows are also invited to lecture on the need for diversity, cultural sensitivity and related topics.
-
The Mosaic Initiative has developed a number of team-building and inclusiveness activities for Division staff, including:
-
Annual Division-wide picnic at Oregon Ridge State Park
-
Annual Multicultural Feast (November) where individuals prepare cuisine from their personal heritage - music and laughter is abundant as well!
-
“Lunch and Learn” sessions on topics such as unconscious bias, racial tension in American cities, religious traditions, art and culture in America
The Division also hosts an annual “Town Hall Meeting” to promote dialogue about a range of issues which might not otherwise have a forum.
-