Table of Contents
- A Message From the President
- Feature Story: VirtualCare Improves Access and Convenience for Patients
- SNAPT Fellowship Addressed Johns Hopkins Community Physicians Nurse Practitioner Shortage with Experienced Candidates
- Patient Outreach Shows Results
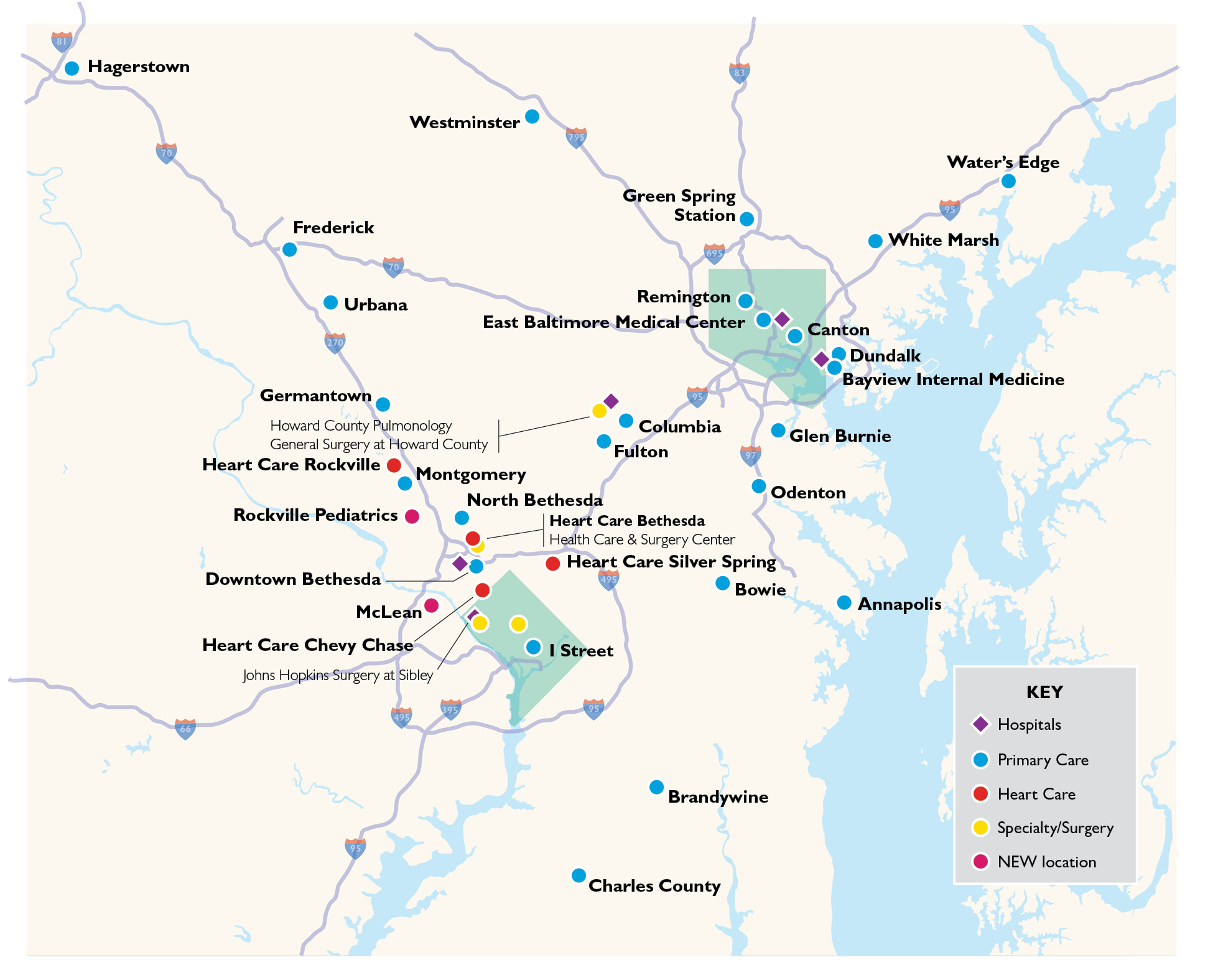
- Feature Story: Johns Hopkins Community Physicians Adds Locations in Rockville and McLean
FY22 By the Numbers
-
50+
Practices
-
902,529
Patient encounters
-
589
Providers
SNAPT Fellowship Addressed Johns Hopkins Community Physicians Nurse Practitioner Shortage with Experienced Candidates
An innovative program to recruit and retain nurse practitioners is showing promise for Johns Hopkins Community Physicians (JHCP).
In response to the nationwide shortage in primary care clinicians, in 2021, JHCP and the Johns Hopkins University School of Nursing launched Supporting Nursing Advanced Practice Transitions (SNAPT).
Nurses can opt for the 12-month fellowship after earning their degrees, with the final six months spent as a newly licensed and credentialed JHCP employee. The first JHCP fellow, Kiah Bond, D.N.P., joined the Odenton practice in January. Two more fellows joined JHCP in 2022, and up to six more may follow in 2023.
“So far, nearly all JHCP-trained SNAPT fellows have either accepted or expressed interest in applying for a full-time position,” says Michael Albert, M.D., chief of primary care clinical innovation at JHCP. “SNAPT allows JHCP to handpick the best of the best practitioners to enhance our provider teams.”
Throughout the program, fellows have specialty rotations, direct experience in the clinical environment, structured coursework and one-on-one mentoring. They graduate ready to enter the workforce with familiarity and the ability to function at a higher level than they would without the program, says Albert. They also learn about JHCP policies, practices and procedures, as well as the Epic electronic medical record platform.
Mirroring the concept of a medical student internship or physician residency, the program aims to provide a guided transition from classroom to clinical practice, setting each candidate up for a successful career.
Patient Outreach Shows Results
A coordinated effort to reach patients in need of wellness visits, cancer screenings and chronic disease management is showing results.
In 2021, Johns Hopkins Community Physicians (JHCP) saw improvements in eight measurement areas chosen for their correlation to patient health. The tracking areas, which were compared to the 2019 numbers so they wouldn’t be skewed by the COVID-19 pandemic, were:
- Breast cancer screenings
- Colorectal cancer screenings
- Controlling high blood pressure
- Diabetic eye exam
- High hemoglobin A1c, indicating poor control of diabetes
- Monitoring nephropathy for diabetes
- Wellness visits, ages 12 to 21
- Wellness visits, ages 65-plus
- Whole health assessments
The quality metrics are among dozens tracked by payers, including the Centers for Medicare & Medicaid Services. They were singled out for attention by Johns Hopkins leadership because they represent a shift in the patient care paradigm that can save lives, says Sujay Pathak, M.D., an assistant professor of medicine and a practitioner based at JHCP’s clinic in the Remington neighborhood of Baltimore.
The improvements were the result of shared efforts to reach patients in multiple ways, including telephone calls, letters and MyChart messages.
Arts at JHCP Provides Community & Creativity
Alice Lee, M.D., lead for the Arts at JHCP program
Alice Lee, M.D., has always relished doodling, writing and listening to music. “If I hadn’t gone to medical school, I would have been an artist or a writer,” says the Johns Hopkins Community Physicians (JHCP) internist/pediatrician, who practices at the White Marsh location.
In 2016, during the annual JHCP practitioner retreat, Lee realized that many other staffers also had creative talents that they might like to share. So, she talked with Steven Kravet, M.D., JHCP president, and in 2017, the JHCP Arts Showcase was born, giving practitioners opportunities to share their artwork, including photography, crafts and even puppets.
Inspired by the success of the Arts Showcase, the following year, Lee debuted Meraki, a printed journal featuring employee poetry, essays, and photography and other artwork. (The word “meraki” is Greek for “labor of love.”)
The showcase and journal, which merged and became virtual in 2020, are key inspirations for Arts at JHCP, a program created in 2022 and funded by the L. Douglas Lee and Barbara Levinson-Lee Professorship held by Kravet.
The program, Kravet says, “fulfills the couple’s wishes for helping JHCP to thrive” by supporting joy and resilience across the organization, particularly at a time of high burnout because of the COVID-19 pandemic.
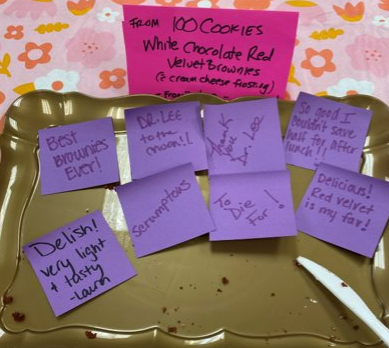
Arts at JHCP hosts activities including book club and baking club meetings, talent showcases and paint nights. Lee, who works with three regional staff liaisons, says their goal is to hold a different event every month, to attract people across the organization with different passions and talents and to foster an improved sense of well-being and belonging in the community.
“My hope is that more staff will be inspired to cultivate a hobby and share their work with colleagues to spread the joy,” says Kravet.
East Baltimore Medical Center Adds Diabetes, Nutrition and Mental Health Support

Expanded health services and lower-cost interventions for patients are two important outcomes from the June 2020 transition of the Johns Hopkins Community Physicians (JHCP) practice at the East Baltimore Medical Center (EBMC) into a Federally Qualified Health Center (FQHC).
By teaming with the Baltimore Medical System (BMS), JHCP tapped federal resources and funds that enable it to offer a broader spectrum of services to an underserved population of 70,000-plus patients.
Since becoming part of an FQHC under BMS, the practice serving the east Baltimore region has added on-site diabetes educators, nutritional services, behavioral/mental health support and case management staffing. Access to both BMS and FQHC supply pipelines allows the practice to offer its patients free or deeply discounted medications and medical devices, such as Nexplanon for birth control and blood pressure monitors.
“It’s always been very hard to care for this patient population that most often doesn’t have the means to find transportation for follow-up referrals, so being able to connect people to needed services in the same building is incredibly important,” says Lenora Jones, JHCP director of clinical operations. The added staffing and coordination also support JHCP efforts to help patients who don’t have health insurance sign up for Medicaid, she says.
Like other JHCP practices, EBMC responded to the COVID-19 pandemic with telehealth options, and introduced negative pressure isolation exam rooms to allow patients under investigation for COVID-19 to receive needed care outside of a hospital setting, including hundreds of COVID-19 vaccinations.
“Our physicians and providers have long-standing relationships with their patients and have really built up the trust over the years,” says Jones. “That’s why, at a time of deep distrust and hesitancy regarding COVID-19 vaccination, we were very successful with our patient vaccination rates.”
I really believe we are living the mission handed to us by Mr. Johns Hopkins, that we are to care for the most vulnerable in our community without regard to class or race.
Lenora Jones, JHCP director of clinical operations
Pediatrician Denisse Mueller, M.D., agrees that the transition of EBMC into an FQHC has been a positive experience for staff and patients alike. “Our partnership with BMS has allowed us to provide much needed services for our community, and we continue to enhance the health and well-being of our families,” she says. “Our ongoing relationship with Johns Hopkins enhances the partnership and allows us to continue to access the support and expertise of The Johns Hopkins Hospital.”
Jones and Mueller plan continued expansion of services in the coming year, including an on-site food pantry, point-of-care HIV testing, greater case management access and a new initiative to test pediatric patients for lead. “I really believe we are living the mission handed to us by Mr. Johns Hopkins, that we are to care for the most vulnerable in our community without regard to class or race,” says Jones.
Expansion of Primary Care Clinical Innovations
Small High Acuity/Risk Panel (SHARP)

SHARP experienced substantial growth in fiscal year 2022, increasing patient enrollment by 30% to more than 1,300 patients and adding two new sites — one in Odenton, Maryland, and the other in the Remington neighborhood of Baltimore — to its existing sites in White Marsh and Hagerstown, Maryland, and at the East Baltimore Medical Center.
The program uses a multidisciplinary approach, with a nurse practitioner working with longitudinal primary care clinicians to support their patients who are at highest risk. SHARP provides these patients with extended visits, increased access, virtual services and care coordination.
“Working with patients who are at a high risk that need more frequent monitoring can help decrease hospital visits and readmissions,” says nurse practitioner Carol Dodson, C.R.N.P., who manages the Hagerstown SHARP program. “The purpose is to see patients in between primary care visits and have more time allotted so complex issues can be managed in a more in-depth manner.” Dodson’s SHARP program is piloting home visits for patients who are at highest risk and bedbound, which she says has proved very beneficial to their care plans. She and her team earned a 2021 Clinical Collaboration and Teamwork Award from the Office of Johns Hopkins Physicians for their work with the SHARP program. The award noted improvement in patients’ health metrics, including a decrease in the average A1C control measure from 22.3% in 2020 to 14.5% in 2021. For this metric, a lower percentage correlates to better care, and this absolute decrease of 7.8% indicates a 54% improvement from 2020.
Johns Hopkins Home-Based Medicine (JHOME)

Johns Hopkins Home-Based Medicine (JHOME) is a primary care program that provides in-home visits for patients age 65 and older who have trouble leaving their home due to chronic conditions such as arthritis, heart failure and dementia. After decades of being part of the Johns Hopkins Bayview Medical Center’s geriatric academic program, JHOME transitioned to the Johns Hopkins Health System in 2019, under the direction of the Johns Hopkins Home Care Group and Johns Hopkins Community Physicians. In 2022, more than 500 patients were served, and the program has nearly 400 active patients. Its staff has also grown to a multidisciplinary team of 16 full-time and part-time clinicians and providers, including geriatricians, nurse practitioners, nurses, care managers and clinical support staff members.
“Because we bring medical care to people in their homes, we help people remain in their homes longer and avoid going to the emergency room or hospital for care,” says Mattan Schuchman, M.D., JHOME’s medical director. When an urgent issue arises, such as problems with urination or trouble breathing, JHOME clinicians can usually treat patients within 24 hours. In 2021, the program earned an Innovations in Clinical Care Award from the Office of Johns Hopkins Physicians, which noted that the program has far exceeded national benchmarks in advanced-care planning and home end-of-life care, and has greatly reduced unnecessary end-of-life hospital and acute care for its patients. Through a partnership with Johns Hopkins Advantage MD, JHOME has demonstrated an overall savings per member per month of roughly $1,500.
In the Community
We have made it a goal to prioritize community engagement. Each fiscal year, teams across our geography hold fundraisers, sponsor programs in their communities and attend local events. See just a few examples of our community engagement from FY22 in the slideshow below.
Heart & Vascular Care — Working Like One Organization
Johns Hopkins Community Physicians (JHCP) cardiology is connected to the Johns Hopkins Heart and Vascular Institute’s cardiology team in myriad ways — from collaboration on complex cases to joint Grand Rounds and quality care improvements. In Fiscal Year 2022, the JHCP Heart Care practices, with offices in Bethesda, Chevy Chase, Rockville and Silver Spring, had 17 M.D.s and one nurse practitioner, and the group plans to add several more physicians and advanced practice providers in the coming years. In addition to complex cases, JHCP and Johns Hopkins University School of Medicine (SOM) cardiologists collaborate in the structural heart realm and on advanced heart failure and adult congenital heart disease. One clinician Zeshan Ahmad, M.D., an electrophysiologist, splits his time, spending 80% with JHCP cardiology and 20% with the SOM cardiology department.
Each month, JHCP, school of medicine cardiology faculty members, and Suburban Hospital and Howard County General Hospital cardiologists join together for a town hall during which the heads of each practice give updates. JHCP cardiology also holds Grand Rounds with Suburban Hospital cardiology, during which a JHCP clinician presents on a clinical topic and a school of medicine faculty member discusses related research.
Additionally, JHCP and SOM clinicians collaborate on quality care improvements regarding congestive heart failure, including standardizing orders, reducing readmission and ensuring early post-discharge appointments for patients. They also work together on quality assurance measures in the cardiac catheterization and electrophysiology laboratories and regarding outpatient echocardiograms and nuclear imaging.