Reverse Total Shoulder Replacement
What is a reverse total shoulder replacement?
A reverse total shoulder replacement is a special type of shoulder surgery. During the surgery, a surgeon removes the damaged parts of the shoulder and replaces them with artificial parts.
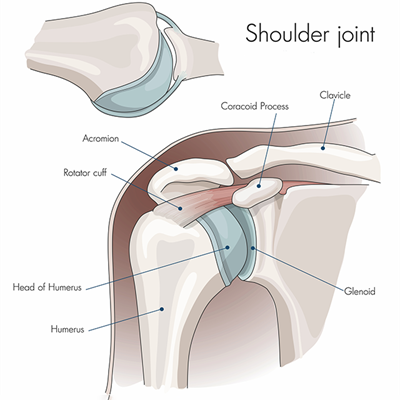
The shoulder joint is made up of the upper arm bone (humerus) and the shoulder blade (scapula). The rounded end (ball or humeral head) of the upper arm bone moves inside a shallow socket in the shoulder blade. Because of this, your shoulder normally has a very wide range of motion. Cartilage, tendon, and ligaments around the joint also provide support and help the joint move smoothly.
What is the difference between a reverse and standard shoulder replacement?
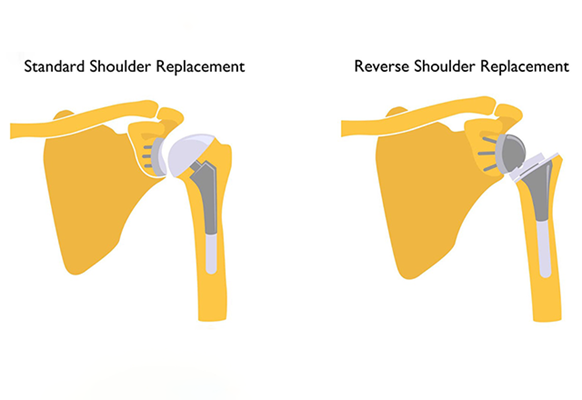
The difference between a reverse prosthesis and a standard shoulder replacement is that in a reverse prosthesis, the ball is placed on the socket side of the joint. This is opposite of where it is located in nature, or “reverse” of what you would expect. The socket is then placed on the arm side where it is supported by a metal stem in the arm bone (the humerus).
In a standard surgery, the metal ball attaches to the upper part of the humerus and the new plastic socket attaches to the shoulder blade. This more closely follows a person’s real anatomy.
Who may need a reverse total shoulder replacement?
Surgery may be an option if you have severe pain that gets in the way of everyday activities. Surgery may also be advised if you have weakness in your shoulder and are not able to move it fully. It may also be advised if your symptoms don’t get better with other treatments, such as medicines, shots (injections), and physical therapy.
Why should a person get a reverse prosthesis instead of a standard shoulder replacement?
Most people get a standard total shoulder replacement. However, a reverse total shoulder replacement may work better for people with certain injuries, including some rotator cuff injuries. This is because a standard total shoulder replacement relies on muscles and tendons around the shoulder joint to be intact, while a reverse prosthesis is designed for situations where the rotator cuff is torn or malfunctioning.
If you have this type of injury, a standard shoulder replacement might still leave you with pain and limited movement. A reverse total shoulder replacement usually improves these problems. After surgery, you can use your deltoid muscle instead of using the rotator cuff to lift your arm.
Reverse Shoulder Replacement | Q&A with Dr. Edward McFarland
A leading expert in his field, Edward McFarland M.D., explains the difference between Total Shoulder Replacement and Reverse Total Shoulder Replacement. An R-TSR can be the solution to certain conditions that a regular Total Shoulder Replacement cannot resolve.
What shoulder conditions warrant reverse total shoulder replacement?
- Rotator cuff tear arthropathy: The most common reason to consider a reverse prosthesis is when there is arthritis of the shoulder joint and the rotator cuff tendons are torn or gone. A reverse prosthesis can significantly reduce pain and restore some range of motion in the shoulder.
- Rotator cuff tears: If the rotator cuff tendons are all torn and a person cannot lift the arm high enough to function, reverse prosthesis could help regain motion and function. When the patient goes to lift the arm there is a prominence on the front of the shoulder. It is called an anterior-superior migration or subluxation of the shoulder. Typically, in this case, the shoulder is not painful but the inability to lift the arm is disruptive to daily life.
- A previous standard shoulder replacement causing lingering symptoms: Healthcare providers may recommend reverse total shoulder replacement to people who have already had a standard shoulder replacement for osteoarthritis, fractures or other reasons. These people may still have symptoms, including pain and loss of motion, that a reverse total shoulder replacement could address. The surgery to place a reverse prosthesis after a standard shoulder replacement was performed is complicated. The existing shoulder prosthesis must be removed before the reverse prosthesis can be placed.
- Shoulder fractures: A person may need a reverse prosthesis for some fractures of the shoulder area, particularly those close to where the ball attaches to the shaft of the arm bone (humerus). In some cases, the bone is broken into many pieces or the ball may be split into parts.
- Proximal humerus tumors: A reverse prosthesis may be necessary due to a tumor in the proximal humerus that involves the bone of the shaft of the bone or the ball of the humerus itself.
Who should not have a reverse total shoulder replacement?
There are only a few instances where a reverse prosthesis cannot be implanted. Sometimes, the socket bone of the shoulder blade or scapula is too far gone to allow fixing of the component base plate with screws. In some instances, a bone graft can be added at the time of surgery, which makes it possible to place the base plate and screws.
Patients with an ongoing infection in the shoulder should not have a reverse prosthesis. However, if the infection can be cleared up then a prosthesis can be inserted. Whenever a shoulder replacement is attempted in a shoulder that has had a previous infection, the post-operative infection rate is higher than if the shoulder never had an infection. This should be discussed with your doctor before the surgery.
What results are possible after a reverse total shoulder replacement?
The reverse prosthesis is good at providing pain relief. Studies from Europe indicate that about 85-90% of patients who have this procedure obtain excellent pain relief. The degree of pain relief depends largely on the reason for the procedure. The degree of pain relief for revision cases is lower than for first-time replacement, and this is believed to be due to the scar formation and long-term damage.
The reverse prosthesis should also restore some range of motion to the shoulder, but the degree of this improvement is not as predictable as pain relief. Most patients can reach the top of their heads without the need to tilt their head. Most patients also see improvement of motion in other directions. However, if the rotator cuff was torn completely, there may not be an improvement in the ability to reach out to the side away from the body (external rotation).
Johns Hopkins Shoulder and Elbow Surgery
Our team of orthopaedic shoulder and elbow specialists diagnoses and treats common and complex shoulder and elbow conditions, including rotator cuff tears, ulnar collateral ligament (UCL) tears, and shoulder and elbow arthritis. Our specialists are also skilled in different shoulder replacement approaches.
Risks and Complications of Reverse Total Shoulder Replacement
Every surgery has risks. The complications of this procedure are similar to those of joint replacements of any joint in the body, and a few complications are unique to reverse prosthesis.
Risks for this surgery include:
- Dislocation of the artificial joint is the most common complication after a reverse total shoulder replacement. The humerus or arm portion (the socket) can become dislodged or disconnected from the ball (the shoulder blade part). This complication is more common with the reverse prosthesis than with regular shoulder replacements. Typically, it can be managed by placing the arm back into the proper place and immobilizing the arm for a period of time. If the prosthesis continues to dislocate then sometimes further surgery is needed to tighten things up.
- Infection occurs rarely but can be frustrating for the patient and physician alike. Sometimes the infection can be controlled by surgery to wash out the joint and with antibiotics. If the infection becomes chronic despite treatment, then there are options for solving the infection, but they largely involve further surgery.
- Excess blood loss. Most patients donate blood before the surgery, which can be given back to them if needed. Only about 10-20% of patients who are having a first-time joint replacement need a blood transfusion, compared to almost 80% of patients who have a revision surgery, which lasts longer.
- Damage to the surrounding nerves (which might impair arm movement). Tingling, numbness and weakness can occur if the nerves to the arm stretched during surgery.
- Break (fracture) of one of the shoulder bones
- Complications from anesthesia or a reaction to certain drugs
- When the arm part of the prosthesis makes contact with the bone of the shoulder blade in certain positions, it can create a groove in the bone of the shoulder blade that usually is not painful. This complication does not typically require surgery and can be controlled by avoiding certain arm positions and with medication.
- Injury to blood vessels is very rare but can happen particularly when there is a lot of scaring, and the patient has had multiple operations.
- Other rare complications include:
- Blood clots in the legs (deep venous thrombosis) which can travel to the lungs (pulmonary embolus)
- Heart attacks
- Strokes
Some of these risks may be higher in people having a repeat surgery. Your risks may vary depending on the anatomy of your shoulder problem and your general health. Ask your doctor about the risks that apply to you.
Preparing for Reverse Total Shoulder Replacement
Talk with your provider about how to prepare for your surgery.
- Tell your provider about all the medicines you take. This includes over-the-counter medicines such as aspirin and all prescription medicines. It also includes herbs, vitamins, and other supplements.
- Ask if you need to stop taking some medicines before the surgery, such as blood thinners.
- Don’t eat or drink after midnight the night before your surgery.
- Follow any other instructions from your healthcare provider.
Before your surgery, you may need imaging tests. These will give your provider more information about your shoulder. These might include:
- X-ray
- CT scan to see the bones in more detail
- MRI to see the soft tissue around the bones in more detail
What Happens During Reverse Total Shoulder Replacement
Your surgeon will explain the details of your surgery. The reverse total shoulder replacement surgery is similar to the regular shoulder replacement, with a few variations. An orthopedic surgeon performs the surgery aided by a team of specialized healthcare providers. The procedure takes several hours. A first-time shoulder replacement typically takes less time than a surgery to replace an existing prosthesis, which can take three to five hours.
In general, you can expect the following:
- You will likely have general anesthesia. This will make you sleep through the surgery.
- You might also get an injection that blocks the nerves in your shoulder and arm. Some people have this instead of general anesthesia.
- A healthcare provider will carefully check your vital signs during the procedure.
- A surgeon makes a cut through the skin near the top of the shoulder, and then cuts through the layer of muscle beneath.
- The damaged sections of the humerus and the scapula are removed.
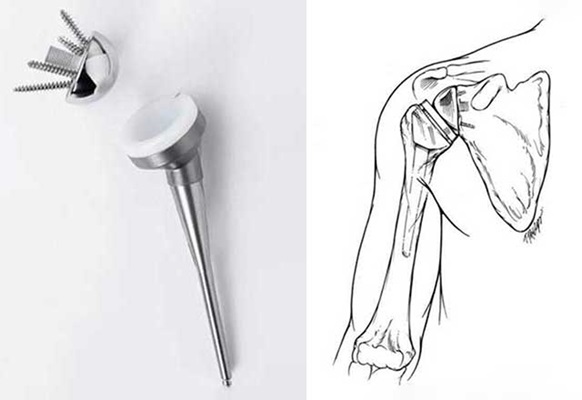
- A metal plate is attached to the socket side of the shoulder joint with screws, which hold it into the bone of the shoulder blade. The ball part of the prosthesis is then screwed into the plate.
- The part of the prosthesis placed into the arm bone is secured with cement, which bonds the metal to the bone within a few minutes. The plastic socket piece is then press-fit into the end of the stem where it is securely fixed by locking into the metal piece. This allows the socket to rotate on the ball so that the shoulder motion can be restored. The muscles around the shoulder also help keep the reverse prosthesis in place.
- The surgeon may place a tube to drain extra fluid in the joint. This tube will be taken out later.
- After the new joint is in place, the surgeon closes the muscles and skin with stitches or staples.
What happens after a reverse total shoulder replacement?
Ask your provider about what you should expect after your surgery. In general, after your operation:
- Your operated arm may be numb from the anesthesia. You also may not be able to move your hands or fingers. This will last for several hours.
- You may have some pain, but pain medicines (orally or by vein) may help as needed.
- You might use a device to keep ice on your shoulder.
- You will probably need follow-up X-rays to make sure your surgery was successful.
- Your arm will probably be in a sling after the surgery for several weeks.
- You will probably begin physical therapy exercises while you are still in the hospital.
- You should be able to have a normal diet as soon as you can handle it.
- You may need to stay in the hospital for 2 to 3 days.
You’ll have some pain as you heal after the surgery, but your original shoulder pain should be improved.
Follow your doctor’s instructions about caring for your shoulder and wound. This might include continued icing of your shoulder and physical therapy. A little bit of drainage from the wound is normal. But let your doctor know if it continues to swell and bleed, or if you have a fever or chills.
Recovery After Reverse Total Shoulder Replacement
The main factor in recovery is whether this is the first (primary) replacement for the shoulder or whether an old prosthesis was taken out during surgery (revision shoulder replacement). The recovery time for gaining function of the arm is longer after a revision surgery than it is after a first-time shoulder replacement. Other factors that influence the recovery time include whether bone grafting (adding bone where it is missing) is done, whether it holds well and how long it takes the bone to heal.
Your doctor will let you know when you will be able to use your hand and arm more fully. Most patients can begin moving the fingers, wrist and elbow the next day. Light work can be resumed within a few weeks.
Whether shoulder motion begins soon after surgery depends on how well the base plate and ball are fixed to the socket by the screws. In a reverse prosthesis, there is some dependence on the bone healing around the base plate and screws. As a result, movement of the shoulder may be halted for a few days to a few weeks. Despite these precautions, most patients are allowed to use their extremity to eat, read or use a keyboard within a few days after surgery. The amount the patient can lift the arm depends upon many factors and each patient is different. The amount of movement allowed by the patient after surgery also depends upon the fixation of the screws to the bone which can be determined at the time of surgery. Lastly, the amount of motion recovered after this surgery also depends upon how much motion the patient had prior to surgery.
Make sure to keep all your follow-up appointments with your provider. Keeping in close touch with your provider can help you have the best possible outcome.
Lifespan of the Reverse Prosthesis
The long-term survival rates (how long it can stay in the shoulder before it starts to loosen and needs to have more surgery) of the reverse prosthesis have been favorable. Most artificial joints will last several years before they need to be replaced.
The reverse prosthesis has been used in France since the 1980s and was approved by the Food and Drug Administration (FDA) in the United States in April 2004. The experience of shoulder surgeons and patients from Europe seem to indicate that the prosthesis will last 15 years about 90% of the time.






