Theodore DeWeese, M.D., the Sidney Kimmel Professor and Director of Radiation Oncology and Molecular Radiation Sciences, was named vice president of interdisciplinary patient care for Johns Hopkins Medicine. He will work with other directors to develop new service lines across the Johns Hopkins system, and will build on the work he helped catalyze to form the highly successful Kimmel Cancer Center multidisciplinary clinics.

Matthew Ladra, M.D., M.P.H., assistant professor of Radiation Oncology and Molecular Radiation Sciences, was named one of Washingtonian magazine’s 40 Under 40. The honor highlights men and women under age 40 who are “shaping local industries.” The magazine calls the winners, “names you should know now—because they’ll be part of the conversation for years to come.” Ladra was selected for running the Kimmel Cancer Center at Sibley pediatric radiation oncology program, a collaborative program with the Children’s National Health System that provides radiation oncology experts and greater convenience for families who live in the national capital region.

Marikki Laiho, M.D., Ph.D., the Willard and Lillian Hackerman Professor in Radiation Oncology and Director of Molecular Radiation Sciences, received the prestigious Harrington Discovery Institute Scholars-Innovator Award. Laiho was chosen for her research on the RNA polymerase pathway, called POL I. It is a critical pathway mutant cancer genes use to communicate with cancer cells and recover from damage caused by radiation treatment. Laiho developed a new compound, known as BMH-21, that disrupts this communication, causing the death of cancer cells.

Ana Kiess, M.D., Ph.D., received the Journal of Nuclear Medicine’s Editor’s Choice Award for her paper on PSMA-targeted α-particle radiopharmaceutical therapy, a new prostate cancer targeted treatment that delivers radiation-releasing alpha particles to cancer cells that have spread throughout the body. The article also highlights the importance of micro-scale dosimetry studies to measure and better understand the amount of radiation the body receives. The journal selected the paper as one of 2016’s top three basic science manuscripts.
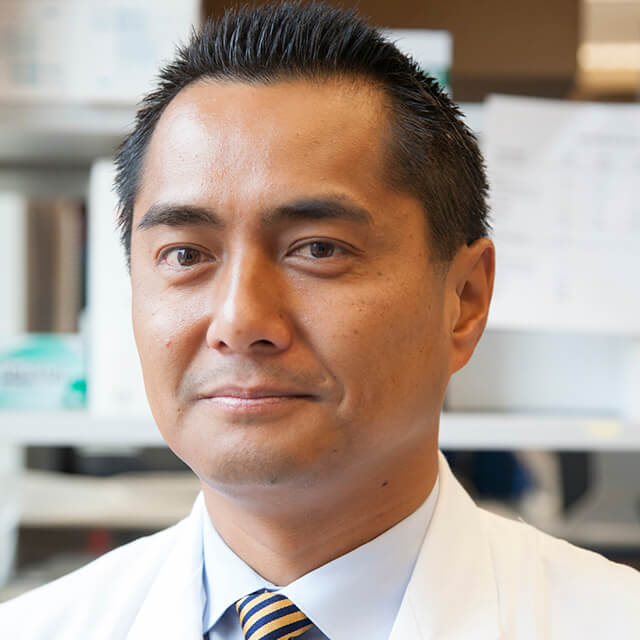
Phuoc Tran, M.D., Ph.D., was appointed clinical director of radiation oncology. Dr. Tran also received a $1 million Movember-Prostate Cancer Foundation Challenge Award to study the stereotactic radiation therapy as an immune stimulating approach to advanced prostate cancer. In 2015, he was also selected for the ASCO Leadership Development Program. Dr. Tran’s research also includes a new approach to salvage radiotherapy for prostate cancer, a mainstay of treatment for men with a persistently detectable PSA or a delayed rise in PSA without evidence of cancer spread. Salvage radiotherapy alone does not always control PSA progression or cure men at highest risk for prostate cancer progression. Dr. Tran is studying whether adding drugs that target the androgen, or male hormone, receptors to salvage radiation therapy will better control prostate cancer and prevent cancer recurrence.
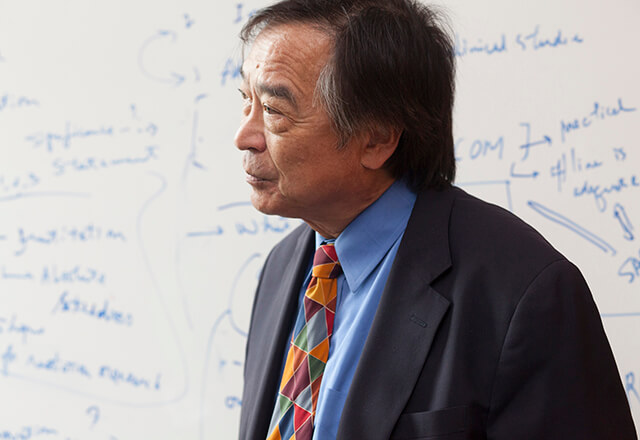
John Wong, Ph.D., director of medical physics, received two prestigious honors. He was awarded the 2017 Edith Quimby Lifetime Achievement Award of the American Association of Physicists in Medicine. In addition, the first conceptual paper on adaptive radiation therapy in Physics in Medicine and Biology, co-authored by Dr. Wong, was selected as one of the journal’s 25 most important papers published in its 60-year history. The paper was featured in the journal’s 60th anniversary collection and was among the papers celebrated at the 50th anniversary of the International Conference on the Use of Computers in Radiotherapy.
Milestones from the Department of Radiation Oncology and Molecular Radiation Sciences
2003: The Department of Radiation Oncology and Molecular Radiation Sciences was established.
2004: IMRT (Intensity Modulated Radiation Therapy) Program began to deliver high-precision radiation that conforms to the three dimensional shapes of tumors and delivers higher and well defined doses of radiation to tumors, and even specific areas within tumors, while minimizing radiation to surrounding normal tissue.

2005: Physicist John Wong pioneered new radiation treatment research methods and models. Dr. Wong constructed miniature versions of the equipment used to treat patients to perform never before done animal research models. These models allow researchers to study the best ways to target radiation-based treatments to tumors and, at the same time, prevent damage to normal cells.
2006: Research by Director Ted DeWeese, M.D., revealed that lower doses of radiation may kill more cancer cells by eluding a protein called ATM, a damage detection mechanism for cancer cells. Researchers are now exploring whether using a drug to block ATM could trick cancer cells into ignoring the damage signals so that radiation effectively destroys more cancer cells.
2007: The stereotactic body radiation therapy program began. This knifeless surgery uses highly focused beams of radiation to ablate tumors.
2008: Molecular Radiation Sciences research accelerated under the leadership of Marikki Laiho, M.D., Ph.D., who began to decipher the biology of DNA-damage response to radiation therapy and how cells sense and repair this damage.
2009: Faculty Advisor Danny Song, M.D., developed a computer-assisted version of brachytherapy, a prostate cancer therapy that uses radioactive seeds inserted in the prostate to kill cancer cells. The innovation allows for more precise placement of seeds. An even more precise version followed, using an MRI-assisted robotic needle to accurately insert the seeds.
2010: An international team of collaborators led by Marikki Laiho, M.D., Ph.D., the Willard and Lillian Hackerman Professor of Radiation Oncology, developed a technique to keep normal and cancerous tissue surgically removed from the prostate alive and functioning for up to a week. This research, which allows investigators to test anticancer drugs on live tissue, is helping experts better understand the biology of prostate cancer and speeding the development of personalized therapies.

2011: Pediatric radiation oncologist Stephanie Terezakis, M.D., led the first-ever in-depth, scientifically based safety analysis of radiation oncology and reported that a combination of several well-known safety procedures could greatly reduce patient-harming errors in the use of radiation to treat cancer. She and collaborators determined that a combination of approximately six common quality assurance (QA) measures would have prevented more than 90 percent of the potential incidents.

2012: Physician-scientist Phuoc Tran, M.D., Ph.D., deciphered the relationship between a cancer growth-promoting gene called c-myc and the ability of cholesterol-lowering drugs called statins to decrease the risk of advanced prostate cancer. In laboratory studies, Dr. Tran showed that high-dose statins reduce c-myc activity.

2013: Marikki Laiho, M.D., Ph.D., uncovered a potential way to stop cancer cells in their tracks. The research focuses on the RNA polymerase pathway, POL I, which is necessary for mutant cancer genes to communicate with cells. In studies using human cancer cell lines, a new, never-described compound known as BMH-21 destroyed this critical communication pathway. These early studies hold great promise because without this transcription machinery, cancer cells cannot recover or function.
2014: In an interdisciplinary research collaboration, Ted DeWeese, M.D., and colleagues revealed that testosterone, a hormone prostate cancer cells need to survive, can also form breaks in the DNA that would make cancer cells more vulnerable to treatment with radiation therapy. The researchers are studying whether short pulses of testosterone, enough to stimulate the breaks but not so much to stimulate the cancer, followed by radiation therapy may cause even more DNA breaks to overwhelm and kill prostate cancer cells.
2015: A unique collaboration between our department of Radiation Oncology at Sibley and Children’s National Pediatric Cancer Center resulted in the first dedicated pediatric radiation oncology program in the National Capital Region. It brings together pediatric medical and surgical oncology experts from Children’s National Health System and pediatric radiation oncology experts from the Kimmel Cancer Center to provide comprehensive pediatric cancer care, including clinical trials, to patients in the region.
2016: The Sidney Kimmel Cancer Center at Sibley Memorial Hospital opened in August adding medical oncology and surgical oncology to the already established and growing Radiation Oncology Program. The 36,000 square foot facility brings patients the most advanced radiation therapy technologies, latest techniques and innovative treatments—the same techniques and technologies used throughout the Johns Hopkins Kimmel Cancer Center.

2017: Akila Viswanathan, M.D., M.P.H., executive vice chair, professor, and director of radiation oncology services for the National Capital Region campus and director of gynecological radiation oncology services for Johns Hopkins brought a pioneering new therapy to the Kimmel Cancer Center. Viswanathan, considered the preeminent expert in gynecologic radiation therapies, developed MRI-guided brachytherapy for cervical cancer and other gynecologic cancers. Johns Hopkins has pledged to continue this one-of-a-kind therapy in her new position.
