The Johns Hopkins Neurosurgical Spine Center is dedicated to relieving pain, restoring function and implementing treatments, including minimally invasive spine procedures, for a wide range of neurologic conditions affecting the spine and spinal cord.
Patient Stories
Paul's Story | Advances in Neurosurgical Spine Surgery
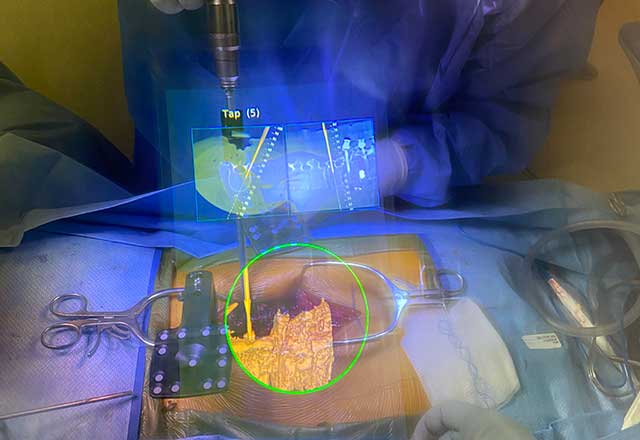
Kay's Story | Augmented Reality Technology
Vivian's Story | Spine Surgery at 95
Appointment Locations
-
Johns Hopkins Bayview
301 Mason Lord Dr.
Baltimore, MD 21224
-
Outpatient Center
601 N. Caroline St.
Baltimore, MD 21287
-
Health Care & Surgery Center - Green Spring Station
10753 Falls Rd.
Lutherville, MD 21093
-
Johns Hopkins Neurosurgery – Bethesda
10215 Fernwood Rd.
Bethesda, MD 20817
Surgery Locations
If spine surgery is needed, it will be performed in a state-of-the-art operating unit in one of our hospitals.
The Johns Hopkins Hospital
1800 Orleans Street
Baltimore, MD 21287

Johns Hopkins Bayview
4940 Eastern Ave
Baltimore, MD 21224

Suburban Hospital
8600 Old Georgetown Rd.
Bethesda, MD 20814

Hear From Our Experts
Approaches to Spinal Fusion | Q&A With Dr. Nicholas Theodore
#TomorrowsDiscoveries: Spinal Fusion Surgeries | Dr. Timothy Witham
Robotic Assisted Spinal Surgery | Q&A With Dr. Nicholas Theodore