Cranioplasty
Cranioplasty is the surgical repair of a bone defect in the skull resulting from a previous operation or injury. There are different kinds of cranioplasties, but most involve lifting the scalp and restoring the contour of the skull with the original skull piece or a custom contoured graft made from material such as:
- Titanium (plate or mesh).
- Synthetic bone substitute (in liquid form).
- Solid biomaterial (prefabricated customized implant to match the exact contour and shape of the skull).
Conventional cranioplasty methods, which have been used by neurosurgeons for more than 100 years, involve peeling back all five layers of the scalp to place the bone remnant or custom implant into the proper cranial location. For the pericranial-onlay cranioplasty, a newer technique developed here at Johns Hopkins by Chad Gordon and his team, the surgeon gently pulls back only the three uppermost layers of the scalp and inserts the bone or implant in between the bottom layers of the scalp protecting the brain. This type of cranioplasty procedure is safer and less invasive.
Why might a doctor recommend a cranioplasty?
Cranioplasty might be performed for any of the following reasons:
- Protection: In certain places, a cranial defect can leave the brain vulnerable to damage.
- Function: Cranioplasty may improve neurological function for some patients. In some instances, a customized cranial implant is designed ahead of time to help the surgeon obtain an ideal shape and outcome, as well as to house embedded neuro technologies.
- Aesthetics: A noticeable skull defect can affect a patient’s appearance and confidence.
- Headaches: Cranioplasty can reduce headaches due to previous surgery or injury.
What does my doctor need to know before my cranioplasty?
Let your doctor know if you:
- Have any health problems, including blood-clotting conditions.
- Take blood thinners such as warfarin, aspirin or anti-inflammatory drugs.
- Have allergies to any medications or other substances.
What happens during a cranioplasty?
In the operating room, you are given a general anesthetic. Once you are asleep, the team positions you so the surgeons have optimal access to the bone defect. The area of the incision is then shaved and prepared with antiseptic, and you are protected by drapes that leave only the surgical area exposed.
You will get a local anesthetic, then the surgeon will carefully cut the skin of your scalp and gently separate it into layers, thereby protecting the dura, which covers the brain. The team cleans the edges of surrounding bone and prepares the surface so the bone or implant can be positioned properly in the defect, after which it is secured to the cranial bones with screws, plates or both.
With the bone or implant in place, bleeding is controlled, the team moves the scalp back to its original position and closes the incision with nylon suture. You may also have a small suction drain left in place to help remove any excess fluid. The drain will be removed in a few days.
What is it like to recover from a cranioplasty?
You will wake up in recovery, and after about an hour you will be transferred to the neurosurgical floor or to the NCCU (neurosurgical intensive care unit). Your nursing staff will continually monitor you for any signs of a complication, and measure your pulse, blood pressure, limb strength and level of alertness. During the first night in the hospital, you will be awakened for these observations.
Operations on the head do not often hurt much, but you may have a headache and will have pain relief pills and injections to ensure you’re comfortable. You may still have a urinary catheter in place from the operation.
In the next day or so, your nurse will remove the IV drip in your arm, and you will be encouraged to walk. Gradually, you will be able to move about normally. Your head bandage will be removed on the second day after surgery.
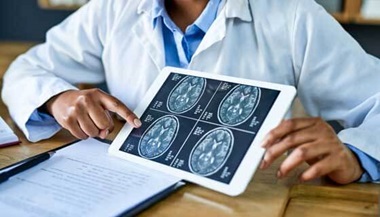
Most cranioplasty patients spend two to three days in the hospital after surgery. When your care team determines you can get around, shower and dress yourself, you will get a repeat CT scan of your head. If the surgical site looks okay, you will be released and can go home.
Skull Restoration with Neuroplastic Surgery | Dennis’ Story
What happens when I leave the hospital?
It may take some time before you feel completely back to normal.
- You will be tired.
- It is common to require a rest in the afternoon.
- You may have intermittent headaches.
- You will schedule appointments for one week and three to four weeks after surgery to have your sutures removed.
- Depending on how quickly you recover from any preoperative disability, you may require rehabilitation.
Contact your surgery team IMMEDIATELY if you notice:
- Increasing headache.
- Fever.
- Seizures.
- Swelling or infection in the wound.
- Fluid leaking from the wound.
Important: DO NOT DRIVE until your doctor says you are ready. You will be assessed a week or two after your surgery to determine if it’s OK for you to drive.
What are the risks associated with cranioplasty?
As in the case of any surgery, you should discuss the risks with your surgeon, including (but not limited to) the following:
- Infection (which may need to be treated with antibiotics).
- Postoperative blood clot requiring drainage.
- Stroke.
- Seizure.
- Clot in the legs (which rarely can travel to the lungs).
- Complication not related directly to the surgery:
- Pneumonia.
- Heart attack.
- Urinary infection.
Johns Hopkins Multidisciplinary Adult Cranioplasty Center | Q&A
Judy Huang, M.D., and Chad Gordon, D.O., discuss a new cranioplasty surgery that can repair the look of indents to the skull after brain surgery, a service offered by the Multidisciplinary Adult Cranioplasty Center.